Knee Extension Strength Assessment: Execution and clinical significance
Available in:
EN
The isometric knee extension assessment is a popular and foundational test in both rehabilitation and performance settings. When assessed with technology-enabled devices such as DynaMo and ForceFrame, it provides valuable insights into knee extensor function, neuromuscular capacity, functional asymmetries and injury risk factors.
This article outlines best practices for knee extension testing in rehabilitation and performance, providing practical guidelines for optimizing knee extension assessment setup to ensure reliable, meaningful data collection.
Knee Strength in Health and Performance
Knee extension strength is a prerequisite for numerous activities across athletic and general populations, including stair navigation, jumping and changing direction. Therefore, quadriceps strength, responsible for producing knee extension moments, cannot be overstated. The following image from the Practitioners Guide to ACL demonstrates the relevance of quadriceps strength in various settings.

…objective measurement of knee extensor performance [gives] practitioners confidence…[to track progress and compare against peers].
Additionally, objective measurement of knee extensor performance provides practitioners with confidence during the rehabilitation plan, knowing how a patient is progressing and how they stack up against their peers.
Standardizing the Isometric Knee Extension
The value of knee extension assessment comes from its ability to generate consistent, reliable data across repeated tests. However, inconsistencies in the practitioner’s setup are a common issue in maintaining accurate, reliable results.
Dynamometers like DynaMo and ForceFrame are externally validated and reliable tools for kinetic assessment. As such, changes in physical outputs can be attributed to one of two variables (Arp et al., 2024; Oxford et al., 2024):
- A change in the setup (e.g., different joint angle or external support, suggesting variability in setup).
- A change in the patient’s capacity (e.g., improved knee extensor strength).
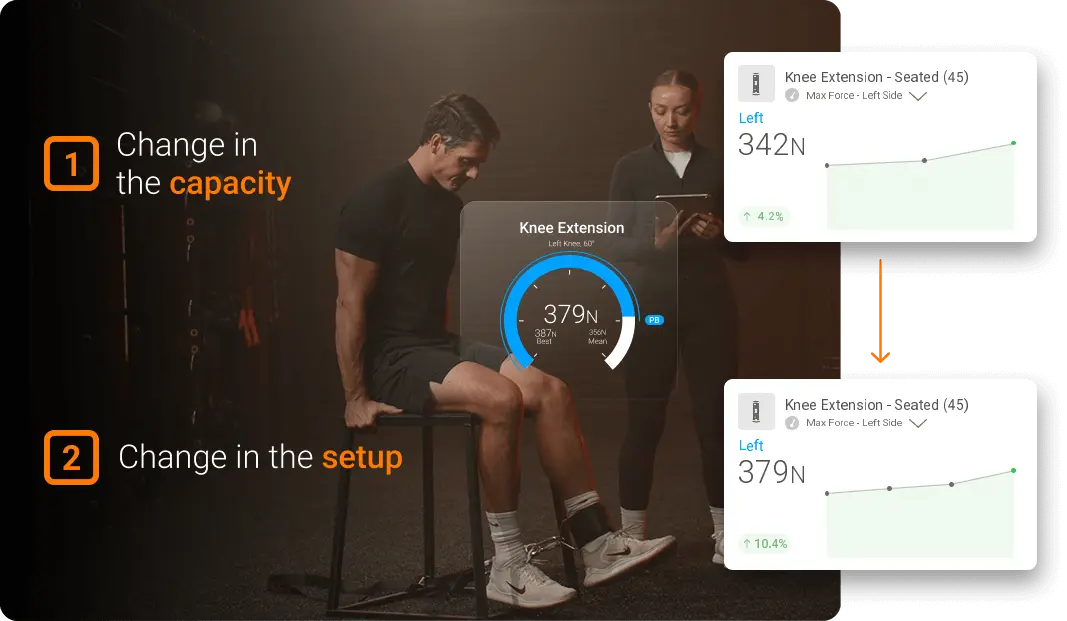
A patient demonstrating improvement in test performance based on two potential factors.
Comparing different setup procedures can be helpful for practitioners to assess knee extensor function (e.g., multi-angle knee extensor profile). However, issues arise when differences in joint angles or setup constraints are unintentional, leading to increased noise in the assessment strategy.
Similar to the squat or drop jump assessments described in other guidelines, clear instructions, consistent positioning and standardized cues are essential for reliable serial measurements.
When utilizing DynaMo or ForceFrame technologies for knee extension assessment, attention to proper setup directly impacts the quality and reliability of your data. The following section outlines key guidelines for proper assessment setup.
Key Setup Considerations
As with many isometric tests, there are key points of performance to consider when assessing a patient’s knee extensor strength:
- Body positioning and constraints
- Equipment positioning
- Pretension
- Testing angles and considerations
Body Positioning and Constraints
Key body positioning and constraints to consider for accurate knee extension isometric testing.
Equipment Positioning
- Seat Height: Adjust to ensure neither leg is touching the ground during the assessment.
- Seat Depth: Adjust depth and padding so the popliteal crease is not compressed against the seat edge. Pinching or compression here will limit the patient’s willingness to give maximal effort.
- Backrest: Set at 85-90° to maximize the stability of the assessment.
- Lever Arm: Align the axis of rotation with the lateral epicondyle of the femur or lateral joint line.
- Pad Placement: Position the pad 2-3cm proximal to the malleoli to maximize comfort while maintaining leverage.
- Stabilization Straps: Secure hips with a seatbelt-like strap to reduce hip-rise, ultimately influencing knee joint angle during the assessment. Chest straps may be necessary for patients with poor trunk control.
- Hand Positioning: Select between secured (e.g., squeezing handgrips near the seat) or unsecured (e.g., arms folded across chest) and maintain consistent execution across serial assessments.
…inadequate stabilization can result in up to 15% overestimation of knee extension strength as patients…change lever lengths to maximize force output.
Research by Krishnan & Williams (2014) demonstrates that inadequate stabilization can result in up to 15% overestimation of true knee extension strength, as patients often inadvertently reorganize by changing lever lengths to maximize force output.
Pretension
DynaMo assessment protocols incorporate a pretension phase to ensure accurate force measurement. However, pretension is just as important for technologies that do not have a pre-built pretension phase. This step helps to optimize the test outcome by doing the following:
- Removing slack from the system
- Minimizing a countermovement, which can ultimately lead to false measures of rate of force development (RFD)
- Establishing consistent starting conditions
Patient performing a knee extension with ForceFrame, demonstrating an adequate pretension phase.
Recommendation: Instruct the patient to kick at ~10% effort to establish pretension.
Consistent pretension helps improve the reliability of metrics like RFD and time to peak force.
Consistent pretension helps improve the reliability of metrics like RFD and time to peak force. However, DynaMo’s “time to 80% peak force (net of baseline)” provides a consistent proxy for assessing RFD when pretension is varied.
Testing Angles and Considerations
Knee extension can be assessed at multiple angles, each with its own advantages and disadvantages. Common testing angles and their significance:
- 45°: Offers a simple and repeatable angle for assessment; helpful during multiple-angle testing.
- 60°: Optimal angle for maximum quadriceps force production; commonly accepted position to test knee extensor strength.
- 90°: A functional position relevant to many daily activities and sporting movements. This makes finding a perpendicular line of pull easier for practitioners. Assesses deeper-range knee strength where ACL strain is minimal.
- Multiple-Angle Testing: Provides insight into angle-specific strength deficits that may not be apparent at any one singular angle in isolation. Commonly performed at 30°, 45°, 60°, 90° and 110-120° of knee flexion.
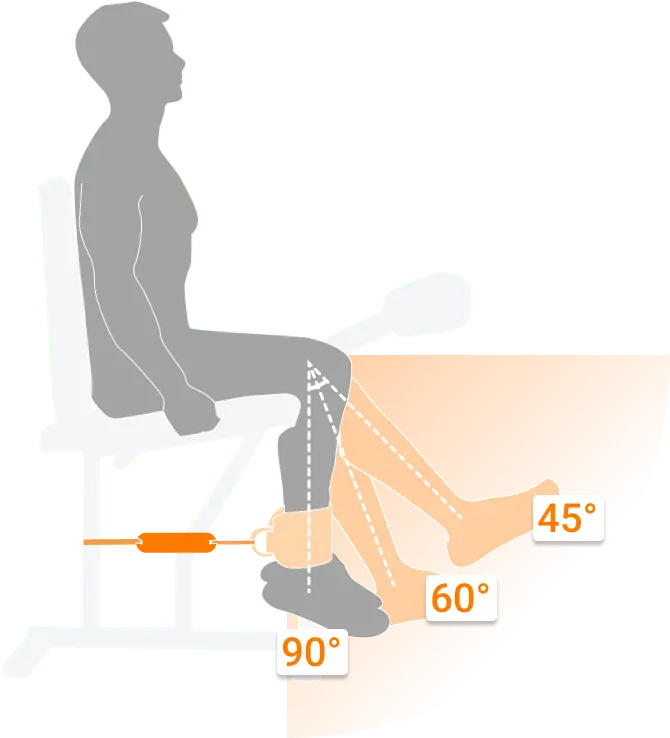
Demonstration of three common testing angles available in the DynaMo App.
…post-ACL reconstruction patients often demonstrate… Greater weakness at deeper knee flexion…
Research by Hart et al. (2022) found that post-ACL reconstruction patients often demonstrate angle-specific deficits. Greater weakness at deeper knee flexion angles often appears even when strength at common testing positions appears normalized.
Metrics to Consider
Leveraging DynaMo and ForceFrame provides access to detailed metrics that go beyond simple peak force values. Key metrics that may prove especially insightful include:
| Metric | Description | Relevance to Practice |
|---|---|---|
| Peak Force | Maximum force produced during a muscle contraction | Indicates maximal strength |
| Mean Force | Average force calculated across multiple repetitions | Provides a reliable alternative to peak force for patients with high variability or when testing strength endurance through long-duration isometric holds |
| RFD (DynaMo Only) | Rate at which force is produced within a given time interval (e.g., 0-100ms) or within a test (e.g., max RFD) | Reflects explosive strength capacity |
| Peak Force Asymmetry (%) | Percentage difference in peak force capacity between limbs | Detects clinically significant imbalances between the left and right sides |
Clinical Applications
The integration of technology-enabled knee extension assessments provides multiple practical applications across clinical and performance settings.
Rehabilitation Focus
- Quantify progress during post-injury protocols
- Identify residual strength deficits following knee injuries
- Guide progressive loading strategies
- Establish objective return-to-sport criteria
- Ensure a patient’s progress is in line with relative norms
Performance Focus
- Inform program design based on specific force-time deficits
- Monitor training adaptations and readiness
- Identify limb asymmetries that may impact athletic performance
- Establish benchmark values for specific sporting populations
Similar to drop jump, countermovement jump and squat assessment, deficits in kinetic performance can persist even when pain and clinical symptoms have resolved. Objective tools such as ForceFrame and DynaMo help practitioners make more informed decisions about progression and return-to-activity readiness.
One of the unique advantages of ForceFrame technology is the ability to transition seamlessly from assessment to intervention. Peak force values obtained during knee extension testing can be used to establish personalized training thresholds in ForceFrame’s Training Mode, specifically targeting strength endurance development.

Patient performing long-lever knee extension isometrics with ForceFrame Training Mode for biofeedback.
Similarly, it is possible to establish threshold values without directly measuring peak forces. For example, in a post-operative setting, typical loading restrictions begin at 10-20% of a patient’s load-bearing capacity. Maximum force can be estimated through pre-injury data, contralateral limb assessment or sport-specific Norms to get an accurate range of performance estimates.
This approach ensures training intensities are individualized and appropriately challenging while remaining within safe parameters. Real-time biofeedback from Training Mode allows patients to maintain target force levels through prescribed durations – a critical component often overlooked in traditional strength and rehabilitation approaches.
Real-time biofeedback…allows patients to maintain target force levels through prescribed durations.
Best Practices for Testing
- Standardize Warm-Up Protocols: Consistency in pre-testing activity ensures reliable results.
- Provide Clear, Consistent Verbal Cuing: “Push as hard and fast as possible” elicits optimal effort.
- Account for Fatigue: Allow adequate rest between trials (minimum 30 seconds for submaximal efforts, 2-3 minutes for maximal efforts).
- Document All Setup Parameters: Record seat position, lever arm length and stabilization methods for future reference.
Conclusion
A well-executed knee extension assessment using dynamometry tools like DynaMo and ForceFrame provides objective, reliable data to guide clinical decision-making. By following standardized protocols for patient positioning, stabilization and testing parameters, practitioners can confidently track changes in quadriceps function throughout the rehabilitation and performance continuum.
The combination of precise measurement technology and standardized testing procedures transforms knee extension assessment from a simple strength test into a powerful tool for injury risk mitigation, rehabilitation progression and performance optimization.
To learn more about implementing DynaMo and ForceFrame in your practice, contact VALD for personalized consultation and training.
References
- Arp, K., Frydendal, T., Kjeldsen, T., Dalgas, U., Timm, S., Viberg, B., Ingwersen, K., & Varnum, C. (2024). Validity, agreement and reliability of the ForceFrame dynamometer in patients with anterior cruciate ligament injury. International Journal of Sports Physical Therapy, 19(9), 1068–1079. https://doi.org/10.26603/001c.122486
- Oxford, S. W., Clarke, N. D., & Tallis, J. (2024). Between-session reliability of field-based assessments of isometric neck strength. Sensors (Basel, Switzerland), 24(15), 5015. https://doi.org/10.3390/s24155015
- Krishnan, C., & Williams, G. N. (2014). Effect of knee joint angle on side-to-side strength ratios. Journal of Strength and Conditioning Research, 28(10), 2981–2987. https://doi.org/10.1519/jsc.0000000000000476
- Hart, L. M., Izri, E., King, E., & Daniels, K. A. J. (2022). Angle-specific analysis of knee strength deficits after ACL reconstruction with patellar and hamstring tendon autografts. Scandinavian Journal of Medicine & Science in Sports, 32(12), 1781–1790. https://doi.org/10.1111/sms.14229
