Finding the balance between prescribing home exercise programs for adaptation and adherence
Available in:
EN
Guest blog by Dr. Sjaan Gomersall, Senior Lecturer in Physiotherapy at The University of Queensland and Clinical Consultant at VALD Performance. Article originally posted to LinkedIn – here.
Exercise is now well accepted as one of the most effective components of rehabilitation, supported by findings from systematic reviews and meta-analyses across a wide range of conditions (O’Keefe et al 2017).
Home exercise programs are a cornerstone management strategy for practitioners working in exercise rehabilitation settings.
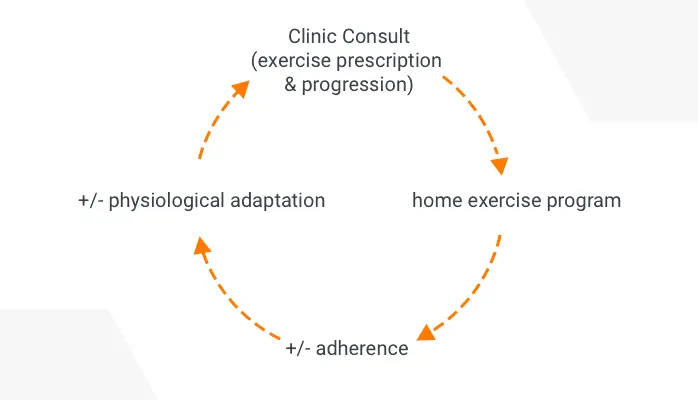
While consultations in the clinic provide opportunities for assessment, passive therapies, education, and exercise prescription, it is the time between visits where clients are asked to complete home exercise programs that are crucial to the client’s treatment outcomes.
Exercise professionals are experts in prescribing exercise rehabilitation programs that are effective for eliciting physiological adaptation in the target system to address the client’s impairments.
Informed by exercise prescription guidelines, experience, and best-evidence, exercise professionals prescribe programs of sufficient frequency, intensity, time, repetitions, sets, and loads in order to elicit physiological adaptation in their clients.
However, the intended physiological adaptations will only occur if clients adhere to their home exercise programs.
Why is adherence so hard to achieve?
Adherence is described by the World Health Organisation (WHO; 2003) as “the extent to which a person’s behavior, which could be taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a health care provider”.
While adherence and compliance can often be used interchangeably, the term adherence has specifically been used here to capture the active role that clients play in their own health care and shared-decision making that underpins the exercise professional and client interactions (Hoffman et al 2020).
Adherence to home-based exercise programs is one of the biggest challenges facing exercise professionals, with average adherence reportedly as low as 30% (Essery et al. 2017).
Adherence is a complex problem that requires a multi-level approach and clients are not solely responsible for their ability to adhere to exercise programs (WHO 2003).
Clients need to be informed, motivated and skilled in order to carry out their home exercise programs, and too often practitioners may run out of time or make assumptions about their client’s motivation or skills, particularly outside of the clinical setting and their ability to transfer any skills taught in the clinic into their unsupervised, home environment.
Promoting adherence requires client-centered and individually tailored strategies to enable clients to adhere to home exercise programs and achieve optimal health-related outcomes.
A combination of evidence-based prescription for physiological adaptation and best-practice strategies to promote adherence is most likely to result in the best possible client outcomes.
What does this look like in practice?
There are many strategies that have been developed and tested with the aim of improving adherence to home exercise programs, as well as a large body of research that has explored the predictors, barriers, and facilitators of adherence in this context.
One example is the use of action planning, which involves prompting your client to make a detailed plan about how and when they will carry out their program – on which days of the week, at what time.
Recently, TeleHab and VALD Health conducted a poll on Twitter asking exercise professionals how they schedule exercises when prescribing a strength program.

Over 60% of respondents reported that they prescribe their programs ‘x’ number of times per week, as opposed to specific days per week, every ‘x’ number of days, or whenever possible.
While ‘x’ number of days per week is in line with exercise prescription guidelines, can we do better to promote client adherence?
In this example, incorporating action planning could see exercise professionals taking some time to help their clients create an action plan for when and how they will complete their home exercise program 3 days per week.
Evidence has shown that action planning can help bridge the gap between intentions to complete exercise and actually carrying out the behaviour, without which we won’t see the desired physiological adaptation.
Ask yourself: Have you tried action planning? What other strategies have you used in the clinic to try to promote adherence to your home exercise programs with your clients?
Interested in learning more about exercise adherence and adaptation?
Check out VALD Health’s two-part webinar series aptly titled; ‘Improving exercise adherence’, hosted by Dr. Sjaan Gomersall and Dr. Simon Lack, Physiotherapist at Pure Sports Medicine and Senior Lecturer at the Queen Mary University in London.
To watch part one
To watch part two
For more webinar content, sign up for the VALD Health Online Series for free – click here.
References
Bassett SF, 2015. Bridging the intention-behaviour gap with behaviour change strategies for physiotherapy rehabilitation non-adherence, New Zealand Journal of Physiotherapy. 43(3): 105-111. doi 10.15619/NZJP/43.3.05
Essery, R, Geraghty, A, Kirby, Yardley, 2017, Predictors of adherence to home based physical therapies: a systematic review. 39, pp 519-534.
Hoffman, TC, Lewis, J, Maher, C, 2020, Shared decision making should be an integral part of physiotherapy practice, Physiotherapy. 107, pp 43-49.
O’Keefe, M, Hayes, A, McCreesh, K, Purtill, H, O’Sullivan, K, 2017, Are group-based and individual physiotherapy exercise programmes equally effective for musculoskeletal conditions? A systematic review and meta-analysis. BMJ Sports Medicine. 51; pp 126-132.
World Health Organisation (2003), Adherence to long-term therapies: Evidence to action. Geneva, Switzerland.
