Accelerated Achilles Rehab: A case study with Cassandra Downe
Available in:
EN
In this Q&A, Cassandra Downe, a physiotherapist at ORKA Performance in Alberta, Canada, shares her experience using a unique and accelerated rehab approach to treating an Achilles tendon rupture.
Using tools like ForceFrame, DynaMo and ForceDecks, Cassandra discusses the case’s challenges and the lessons she learned.
Can you provide a background about the case?
The patient in this case happened to be an orthopedic surgeon – she was in her early 30s and had ruptured her Achilles tendon during a recreational tennis match. She described the classic symptoms: trying to project forward and up while feeling a big “pop” and the sensation that someone had kicked her in the back of the leg.

A tennis athlete demonstrating the high demands of the calf and Achilles complex in tennis.
After the diagnosis, it was decided that she was eligible to trial an accelerated rehab protocol, as she was moving to Australia in four months to continue her career in orthopedics.
…it was decided that she was eligible to trial an accelerated rehab protocol, as she was moving to Australia in four months to continue her career in orthopedics.
The goals we set out together were directed in part by the patient’s clinical knowledge, the head surgeon’s reports and my robust understanding of Achilles rehab and return to function.
She needed to regain basic ankle and lower leg function quickly, normalize her gait mechanics and prepare for long hours standing in surgery, a primary occupational requirement. This made the early stages of rehab critical for her overall recovery and ability to meet her professional demands.
…the early stages of rehab [were] critical for her overall recovery and ability to meet her professional demands.
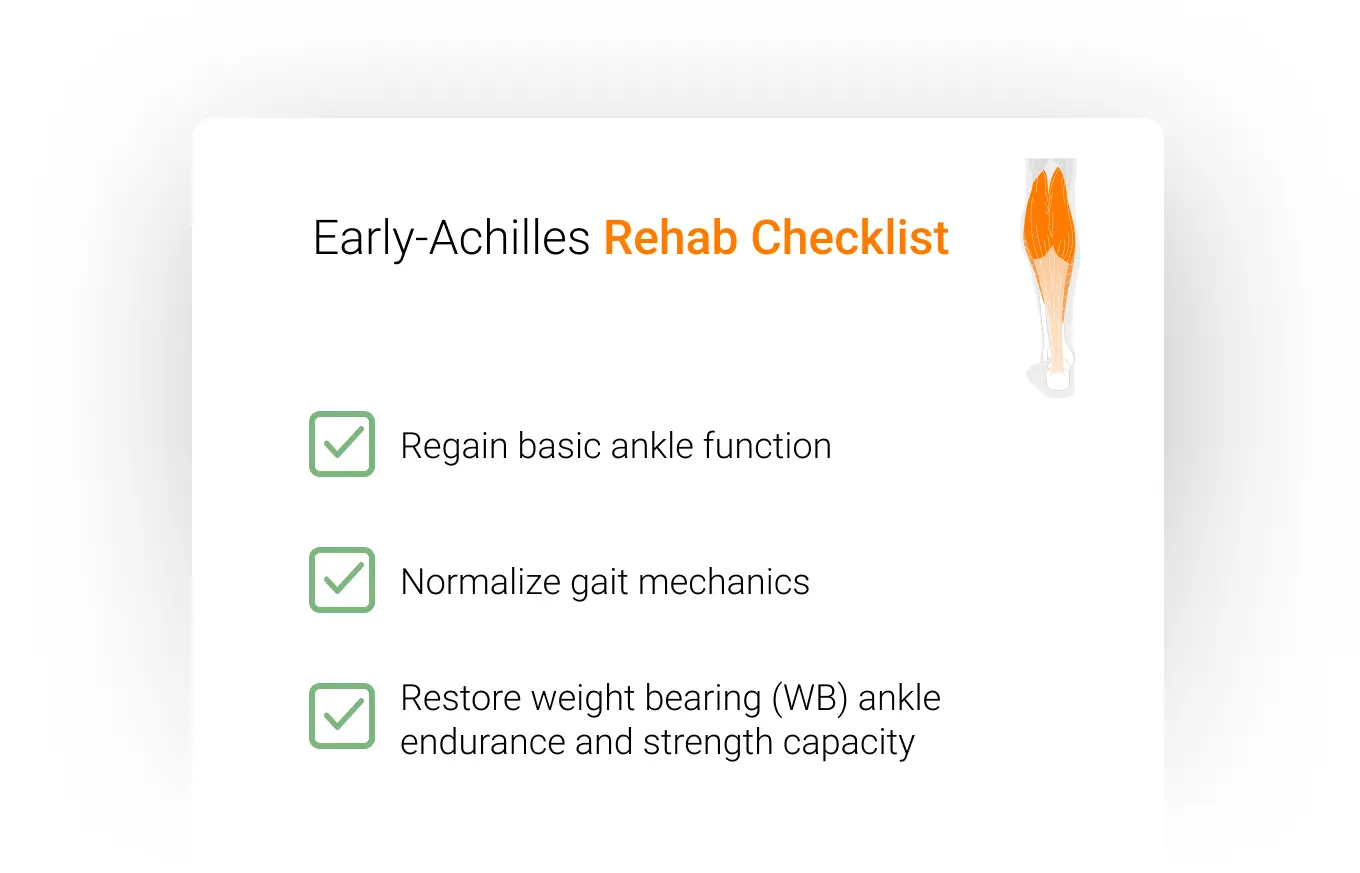
What restrictions were in place in early rehab, and how did you work within them?
With an Achilles rupture, restrictions are put in place to prevent complications like tendon elongation or re-rupture. We implemented an “accelerated” protocol for her rehab, so while we could introduce early loading, it had to be controlled within her surgeon’s guidelines.
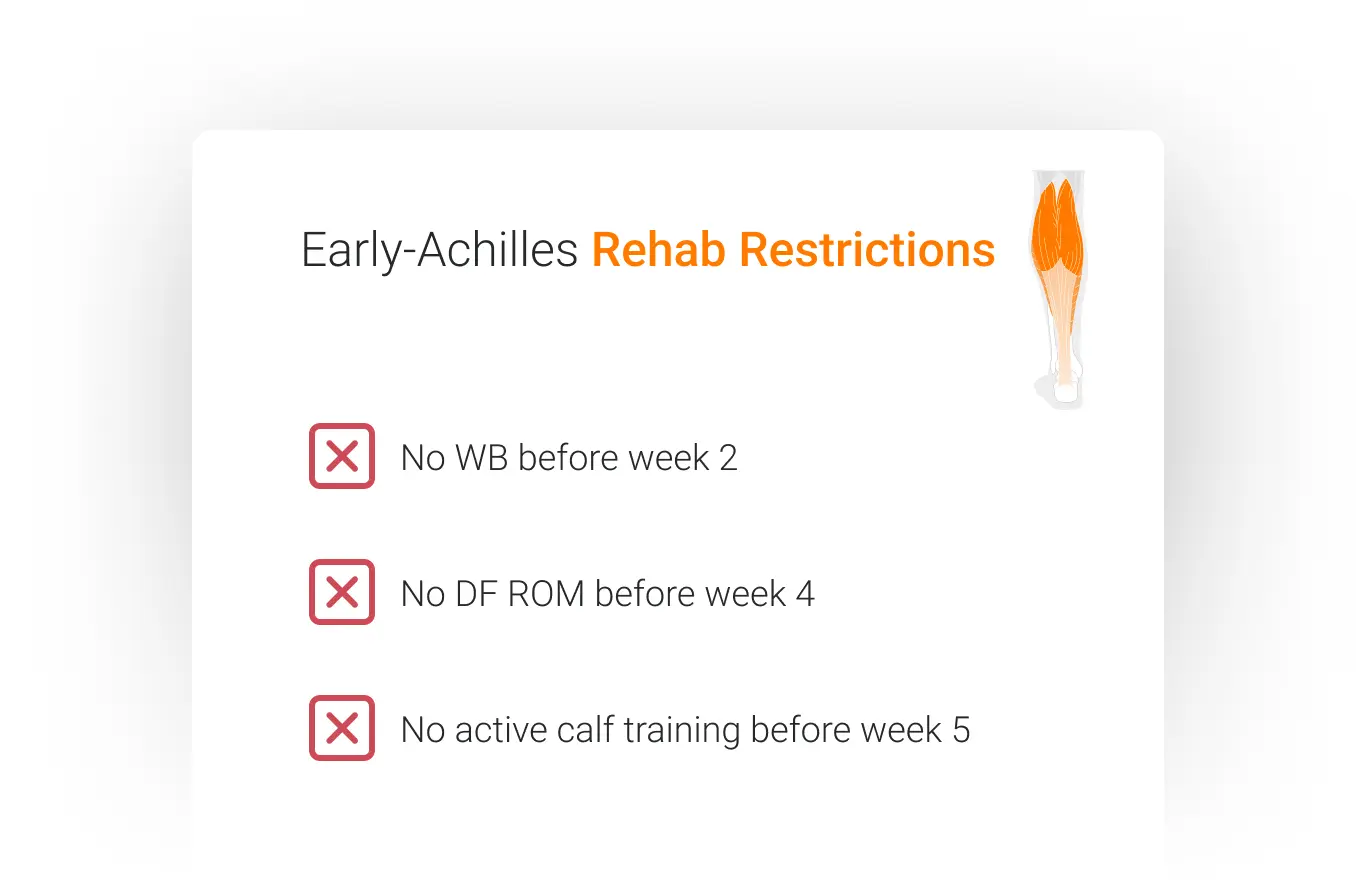
The surgeon provided the following parameters for WB and DF range of motion (ROM) guidelines:
- Weeks 0-2: Non-weight bearing (NWB), with crutches and heel wedges in a controlled ankle motion (CAM) boot.
- Weeks 2-6: Gradual WB progression with set targets (e.g., % body weight each week). DF ROM was progressed to neutral.
- Weeks 6-12: WB as tolerated, with a slow weaning off heel wedges.
The highest risk for re-rupture after Achilles repair occurs between weeks 4 and 12. Therefore, this period was monitored closely for swelling and pain, as well as how specific movements and loads affected her Achilles tendon.
…between weeks 4 and 12 [she] was monitored closely for swelling and pain, as well as how specific movements and loads affected her Achilles tendon.
Luckily, we were able to gather a lot of data, even in the early stages of her rehab.
What technology did you implement during rehab?
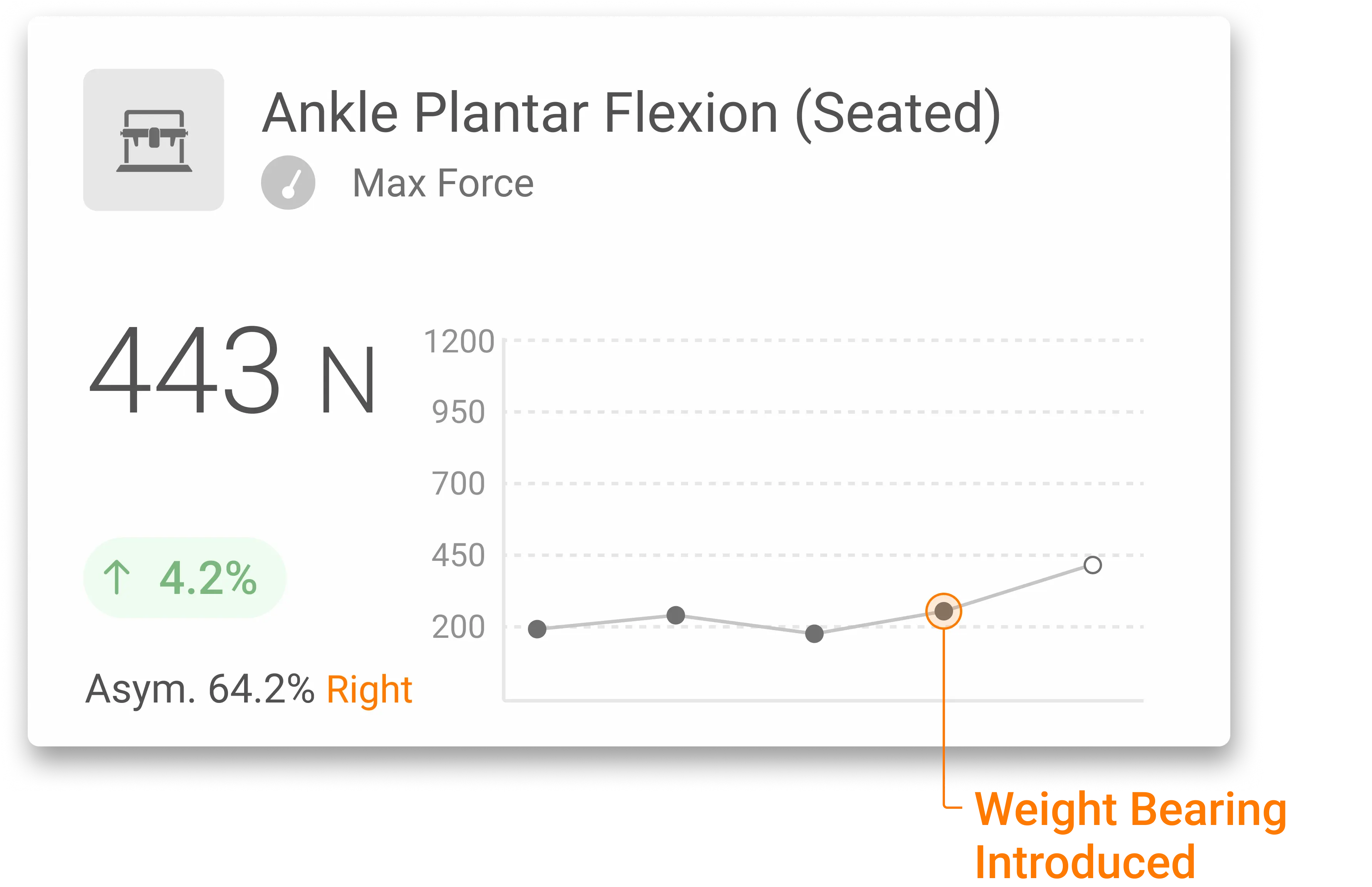
We used ForceFrame – primarily in Training Mode – to set safe load thresholds based on her restrictions. For example, we calculated her peak force on the unaffected side and set a training target at 30% of that value with a 10% variance.
[Using ForceFrame], we calculated her peak force on the unaffected side and set a training target at 30% of that value with a 10% variance.
Over the first six weeks of loading, she could visually track her progress with metrics like time in zone and total impulse while staying within her surgical limits.

We were able to maximize the adaptations she was getting in rehab with BFR training (e.g., AirBands). This allowed us to get a head start on mitigating the negative effects of surgery (e.g., atrophy, decreased rate of force development (RFD) and decreased strength).
How did this approach differ from a traditional Achilles rehab protocol?
Traditionally, Achilles rehab is much more conservative, with the NWB phase lasting six to eight weeks. This can delay muscle activation and tendon loading, leading to stiffness, atrophy and other complications.
However, new research has shown no difference in long-term negative consequences in tendon health between conservative and early-loading protocols when executed correctly.¹
…new research has shown no difference in long-term negative consequences in tendon health between conservative and early-loading protocols when executed correctly [and] multiple benefits.
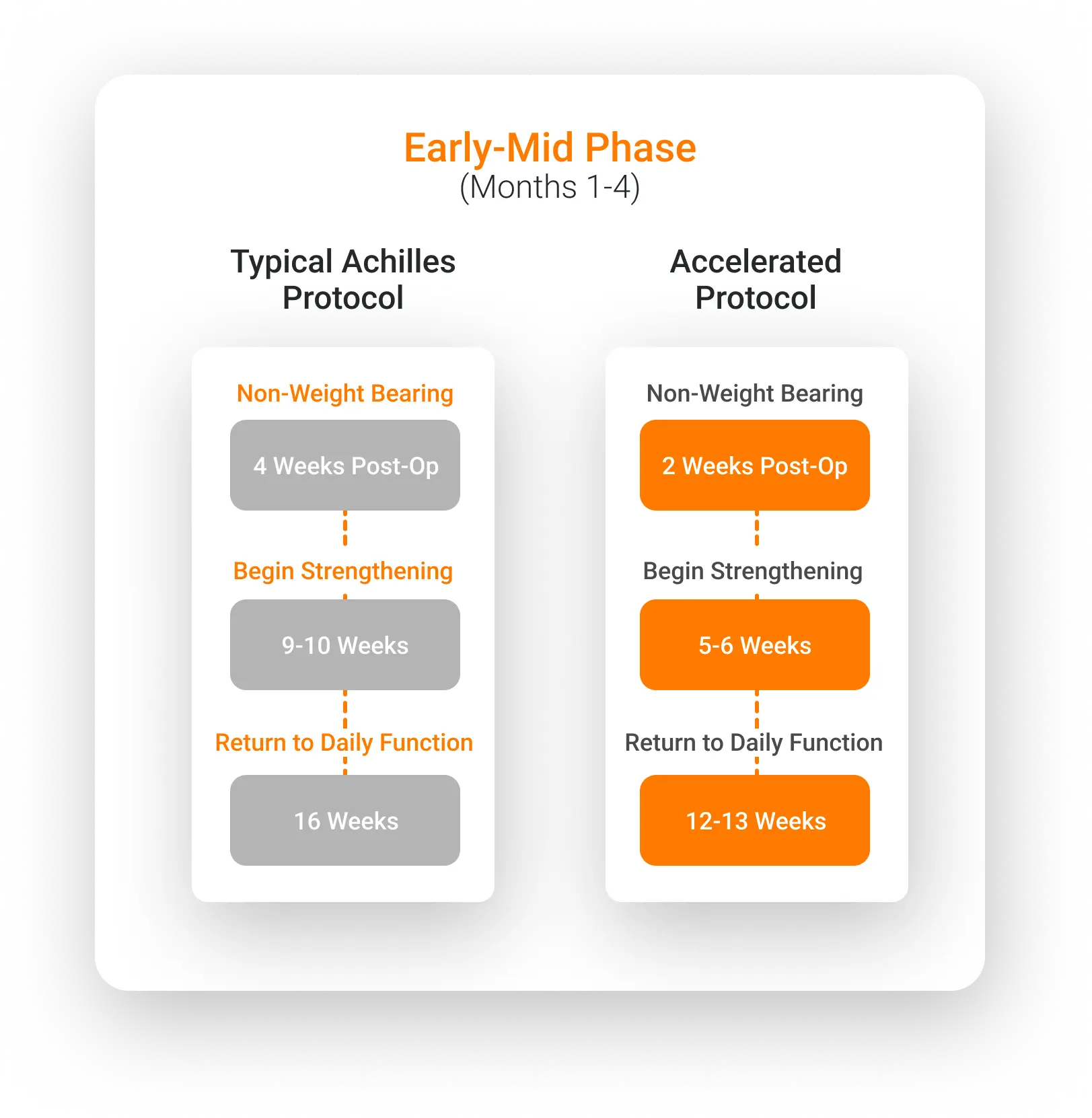
With an accelerated approach, we saw multiple benefits:
- Engagement: The client was highly motivated because she felt like she was actively participating in her recovery.
- Fewer Complications: More activity early on meant her joints and tissues were moving, reducing stiffness and limiting the time needed for passive interventions, such as manual therapy.
- Efficiency: By week six, she was consistently maintaining loads at 30% peak force thresholds and was ready to begin walking at full WB under her surgeon’s discretion.
What were the outcomes of the rehab process?
Upon departure for Australia (16 weeks post-surgery), the client had met all her medium-term goals:
- She was ambulating comfortably with a normalized gait.
- She tolerated standing for long hours during surgeries.
- She reintroduced loaded strength training and was ready for the next rehab phase.
As a surgeon herself, the patient loved the data she got from the technology we implemented. She appreciated how ForceFrame metrics anchored her subjective feelings to objective progress. Interestingly, her progress wasn’t linear.
While there were steady improvements, she also experienced significant jumps in performance, specifically when we transitioned from partial WB to full WB.
As a surgeon herself, the patient loved the data she got from the technology…how ForceFrame metrics anchored her subjective feelings to objective progress.
Looking back, is there anything you’d do differently?
This was my first time implementing this protocol. Initially, I was cautious due to the higher re-rupture rates in weeks 4-12, leading me to lean more on subjective advice from the surgical team about timelines and limitations. With hindsight, I’d approach the early stages with more confidence and fine-tune the progression even further.
Now, having seen the benefits of integrating tools like ForceFrame early on, I’m more comfortable applying these strategies to other cases. The combination of real-time data, patient engagement and advanced technology has reshaped how I approach many post-surgical cases.
Final Thoughts
Cassandra Downe’s innovative approach highlights how technology can drive better outcomes, even in accelerated rehab protocols. By combining clinical reasoning with data-driven tools, practitioners can enhance patient engagement, minimize complications and achieve remarkable results.
If you would like to learn more about integrating VALD’s human measurement technology into your organization to enhance athlete profiling, monitoring and data-driven decision-making, please reach out here.
References
- Okoroha KR, Ussef N, Jildeh TR, et al. Comparison of tendon lengthening with traditional versus accelerated rehabilitation after Achilles tendon repair: a prospective randomized controlled trial. Am J Sports Med. 2020;48(7):1720-1726. doi:10.1177/0363546520909389
