Dynamometry for Achilles Tendinopathy
Available in:
EN
Achilles tendinopathy is a prevalent musculoskeletal (MSK) injury that commonly affects athletes, particularly those engaged in activities that involve high degrees of running and jumping, which apply large magnitudes of load to the Achilles tendon. However, it is important to note that this injury does not develop exclusively in active individuals; up to 65% of diagnosed cases in general practice settings are found to occur in individuals aged 41-60 years and are considered unrelated to sporting or high-intensity activities. (18, 20)
…up to 65% of diagnosed cases in general practice settings are found to occur in individuals aged 41-60 years and are considered unrelated to sporting or high-intensity activities.
My previous guest insight article explored a proposed battery of force plates tests for Achilles tendinopathy, aiming to improve our clinical decisions and treatment outcomes.
While the utility of ForceDecks is not exclusive to active populations, this test battery may be viewed as part of a “progressive functional test approach,” which may inform our clinical assessments and rehabilitation programming for those progressing toward the higher end of the functional spectrum.
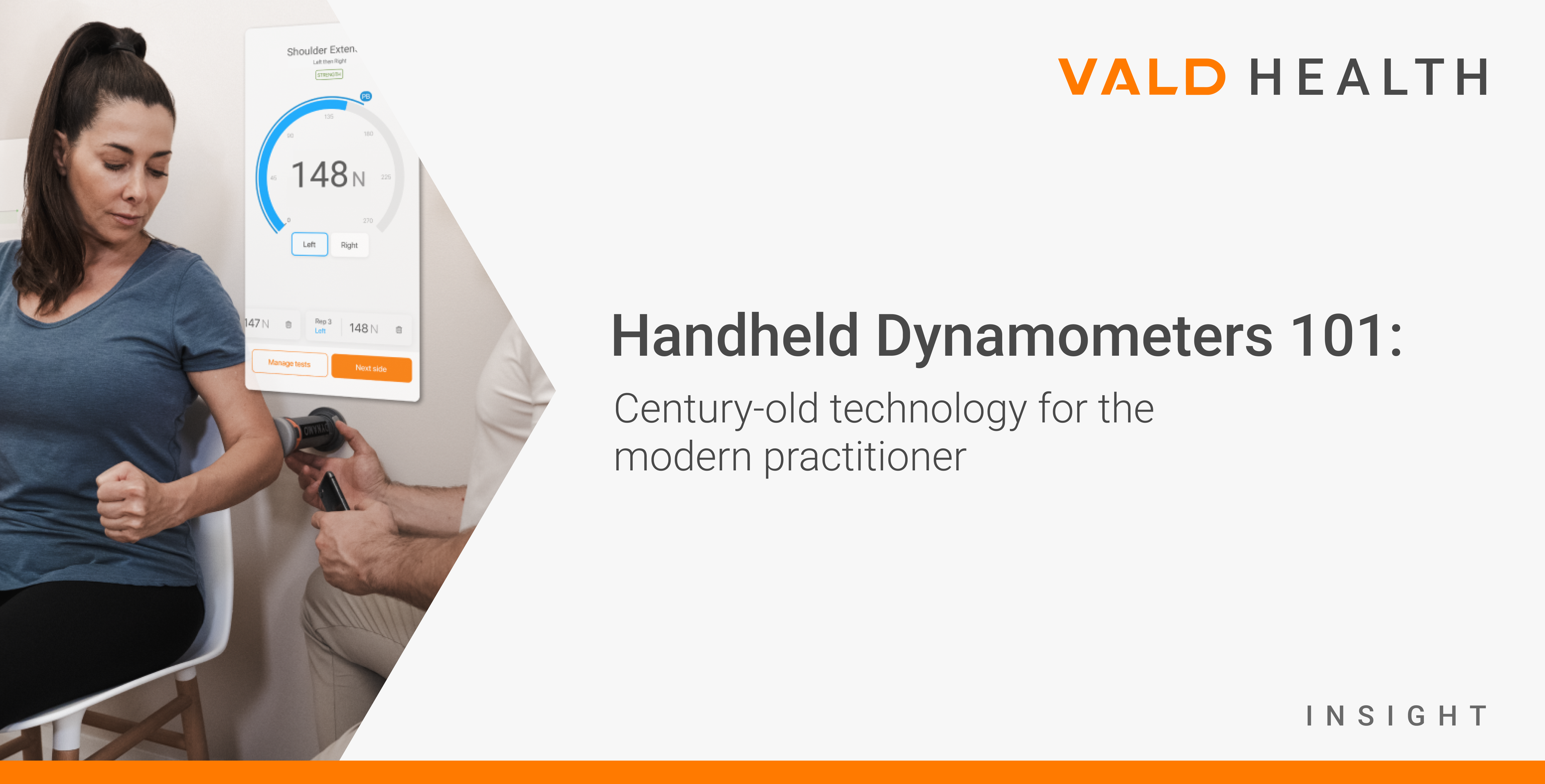
Expanding on the progressive functional test approach described above, the purpose of this article is to explore the clinical utility of dynamometry for assessing the lower end of the functional spectrum, where we may be dealing with clients with a lower initial level of function, a lower capacity goal or those for who we need to isolate specific muscles to inform our clinical decisions.
Ideal Use Cases for Dynamometry

On the Move
When traveling (e.g., at-home treatment sessions, away games with sporting teams) and when larger devices can’t be easily transported.

Efficiency
When a wide range of tests must be performed in a short period of time by a single practitioner (e.g., upper extremity, lower extremity, range of motion (ROM) and more).

Single-Joint Testing
HHDs are best suited for single-joint tests, where forces are typically lower and positions can be easily controlled, either in fixed-point or handheld configurations.

Bed-Based Testing
When the patient must be tested on a treatment bed due to compromised mobility or surgical recovery.
Adaptability
When the test you wish to perform cannot easily be conducted with other isometric testing technologies, such as grip strength, pinch and finger assessments.

Low Force Tests
When the patient is not strong enough to overpower the practitioner or the test produces low forces, HHDs may be the most convenient testing solution.

Accuracy
While accuracy is always important, the added precision, reliability and features of more advanced technology are not always necessary for all users, tests and settings.

Budget Constraints
HHDs are typically the most affordable isometric testing technologies.
Firstly, in this article, “dynamometers” will refer to Fixed-Frame Dynamometers (FFDs), Fixed-Point Dynamometers (FPDs) or Handheld Dynamometers (HHDs).
Functional Assessment Progressions in Achilles Tendinopathy
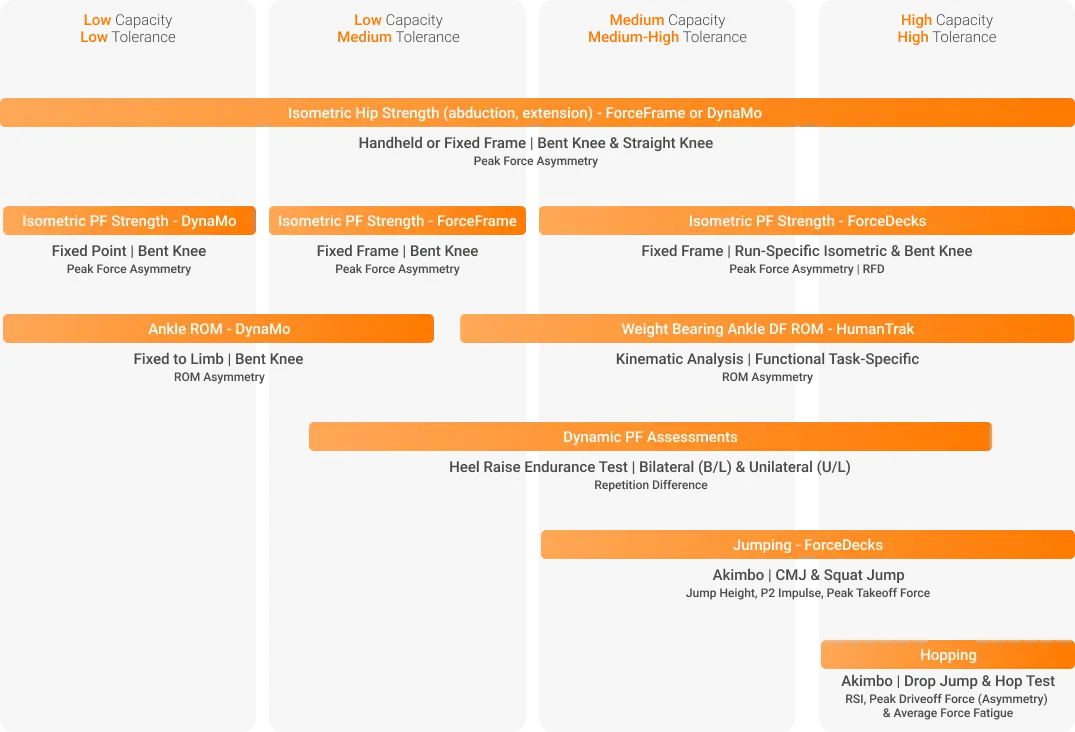
The test continuum below expands on the previously described functional test battery for Achilles tendinopathy. Using dynamometry can greatly assist clinicians by isolating and identifying strength and functional deficits that may form part of an individual’s clinical presentation, not otherwise discernable when utilizing standard manual muscle testing (MMT) methods or more global functional assessments.
When it comes to assessing function in Achilles tendinopathy, the question isn’t “Should we do it?” it’s “What functional tests should we perform?”
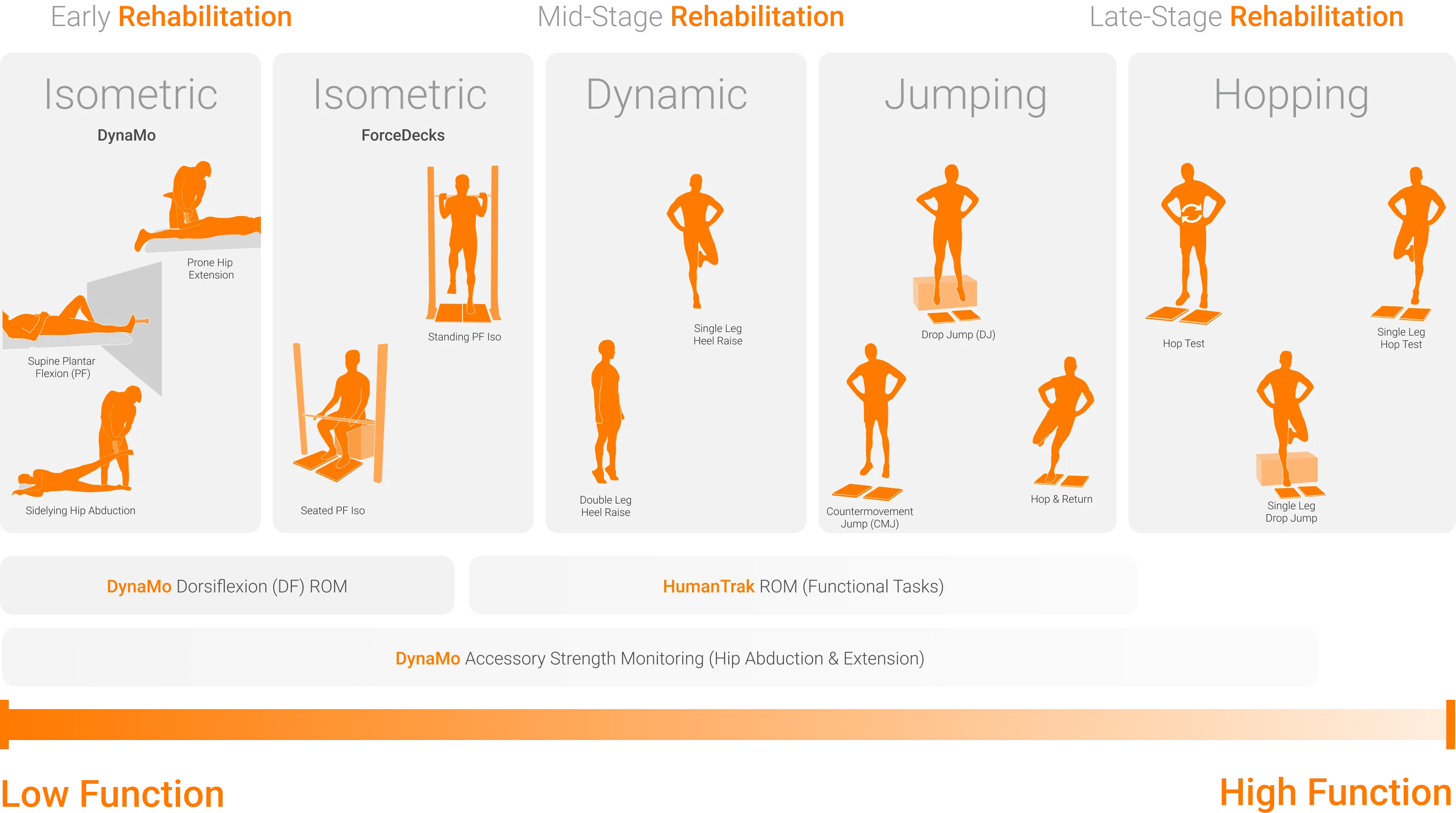
Developing a framework for accurate assessments appropriate to an individual’s stage of recovery and clinical needs helps avoid the “floor and ceiling effect.” This approach ensures that our therapeutic interventions align with an individual’s current capacity and build towards their desired capacity. It’s one thing to know which functional tests we can perform as part of our clinical assessments; however, we need to understand why these tests matter.
It’s one thing to know which functional tests we can perform as part of our clinical assessments; however, we need to understand why these tests matter.
Common Functional Deficits and Assessment Methods Utilized in Achilles Tendinopathy Assessments
In both active and sedentary cohorts, muscle power, strength deficits and reduced DF are considered modifiable risk factors for the development of Achilles tendinopathy. (26)
It is important to recognize that there is still conflicting evidence regarding the predisposing nature of these deficits and their link to developing Achilles tendinopathy in uninjured individuals. (28) However, in the presence of pathology, assessing and addressing these functional deficits are considered important, especially when we identify deficits relative to normative values and asymmetry between limbs. (33)
Identifying and understanding strength or ROM deficits will influence the selection, timing, dosage and progression of our exercise and treatment interventions.
| Deficit | Evidence | Assessment Method | Metric | Therapeutic Interventions & Clinical Decisions |
| Non-Weight-Bearing Ankle DF ROM (5, 18) Weight-Bearing Ankle DF ROM | Varied evidence regarding reduced ROM being a universal risk. | DynaMo HumanTrak DynaMo | ROM Asymmetry | Therapeutic GoalsImprove ankle DF ROM. Interventions to work within ankle DF restrictions if the range is an irritant (e.g., temporary use of heel lifts). Clinical DecisionsE.g., footwear recommendations, advice relating to hill walking, exercise selection and “dosage.” Improve ankle DF ROM. |
| Ankle PF Strength (Isometric) (5, 6, 7, 9, 12, 13, 16, 18) | Gastrocnemius may account for 3.7% to 11% of deficits. Soleus may account for 23.2% to 36.7% of PF strength deficits. (5) | DynaMoForceFrameForceDecks | Peak/Max Force Rate of Force Development (RFD) Time to 80% Peak Force Asymmetry | Exercise interventions via the ability to isolate soleus vs. gastrocnemius muscle influence. Clinical DecisionsE.g., prescribing seated calf strength exercises to target soleus strength deficits (isometric → isotonic → plyometric). |
| PF Dynamic Strength | PF Isotonic Strength and Power. Limb symmetry (18) | Number of Reps (Asymmetry) External Load | Treatment Decisions E.g., tolerance for isotonic movements. Movement ProgrammingE.g., dosage (goal sets-reps and tempo). | |
| Hip Strength Hip Abductors Hip External Rotators Hip Extensors (5, 12, 21) | - | DynaMo ForceFrame | Peak Force Peak RFD (DynaMo) Peak Force Asymmetry | Exercise interventions to target and address hip muscle strength deficits – suitable for both early- and late-stage strength assessments:Low load/early-stage strength: Clams or glute bridges.Higher load/late-stage strength: Maximum voluntary contraction (MVC) isometric hip abduction or Trap-Bar Deadlift. |
Dynamic and Functional Strength
For a comprehensive overview, please refer to this article: Assessing Achilles Tendinopathy with Force Plates.
| Deficit | Evidence | Assessment Method | Metric | Therapeutic Interventions & Clinical Decisions |
| Stretch-Shortening Cycle (SSC) Function (18, 9, 16) Slow SSC Function >250ms | Symptomatic limb associated with lower CMJ height. (7) | ForceDecks CMJ | Jump Height – Impulse-Momentum (IMP MOM) P2 Concentric Impulse | Exercise selection and progression. Return to mid-load activities. |
| SSC Function (18, 12, 9, 7, 16, 6) | Side-to-side differences in drop CMJ height are significantly associated with Achilles tendon peak forces and average loading rates during running. (7) | ForceDecks DJ | Reactive Strength Index (RSI) Peak Drive Off Force Asymmetry Jump Height | Exercise selection and progression. Return to higher-load activities (e.g., jumping, ↑ running pace). |
| Jumping Fast SSC <250ms | - | ForceDecks “Jumping” (Hop Test) | Average RSI Average Peak Drive Off Force Asymmetry Average Force Fatigue | Exercise selection and progression (↑ velocity of movement, etc.). |
| Hopping | Performance deficits of 16% to 35% in individuals with Achilles tendinopathy. (9) Average and maximal hop height deficits of 18% & 16% respectively. Reduced hopping quotient of 20% of symptomatic side. (9) | ForceDecks Single Leg Hop Test | Average RSI Average Peak Drive Off Force Asymmetry Average Force Fatigue | Return-to-sport. Introduce higher-intensity running or jumping (e.g., pace, etc.). |
Purpose of Progressive Functional Assessments and Rehabilitation
As mentioned earlier, when conducting clinical assessments, we must ensure that the methods by which we assess an individual align with their functional capacity and allow us to capture meaningful data. This data will inform our clinical decisions, for example, exercise prescription and loading advice.
Failing to recognize the strengths and limitations of potential assessment methods and clinical interventions, often demonstrated by the “floor and ceiling effect,” can sell our clients short of achieving their functional restoration goals.
“Ceiling or floor effects occur when the tests or scales are relatively easy or difficult such that substantial proportions of individuals obtain either maximum or minimum scores and that the true extent of their abilities cannot be determined.” Liu (2018)
This concept is recognized in current literature and clinical practice, where in 2022, we saw the introduction of the VISA-A (sedentary) patient-reported outcome measure (PROM) to cater to the floor effect experienced by sedentary individuals completing the standard VISA-A, as well as the TENDINS-A introduced in early 2024. (24, 35)
Recognizing the limitations of the clinical assessments and therapeutic interventions we utilize in clinical practice is a strength, not a weakness.
Recognizing the limitations of the clinical assessments and therapeutic interventions we utilize in clinical practice is a strength, not a weakness. The strength comes from knowing when, where and why an assessment or therapeutic intervention has utility and where its limitations lie.
In the context of performing isolated strength testing, MMT remains the predominant (strength testing) method in clinical practice. Despite several well-known limitations of this assessment method. (22)
…MMT remains the predominant (strength testing) method in clinical practice. Despite several well-known limitations of this assessment method. (22)
Demonstrated limitations in utilizing MMT for assessing lower extremity strength include: (22)
- Inadequacy of MMT for measuring forces generated by larger muscle groups, especially in the lower extremity.
- Ceiling effect in which many people attain maximal strength scores, despite sub-clinical deficits in strength, when assessing via MMT. Furthermore, the ceiling effect of MMT limits the ability to detect changes in muscle strength over time.
While using dynamometry is an appropriate next step to mitigate the issues of reliability and accuracy, it is important to note that not all dynamometry assessments are created equal. While assessments like the supine PF assessment have shown to be valid and reliable in some populations, the test results are drastically lower than that of fixed frame and force plate assessments, likely demonstrating a ceiling effect. (36, 32) If possible, fixed frame and fixed-point dynamometry assessments are encouraged to measure the true force-generating capacity of the plantar flexors.
Factors Contributing to Achilles Tendinopathy Injury Recurrence
- Returning to sport too soon. (12)
- Failure to address deficits in musculotendinous function. (12)
- Clinicians fail to formulate individualized rehabilitation programs that address identified deficits relating to the presenting pathology and the physiological demands of the goal activities. (13)
When we appreciate the strengths and limitations of manual clinical assessment methods and consider the often-modifiable factors listed above that may contribute to poor rehabilitation outcomes, the clinical utility of objective testing becomes clear.
Given the evolution of technology, evidence and best practices, the question is not so much, “Why utilize data-driven assessments in my clinical practice?” but “Which data-driven assessments best suit my clinical practice?”
Floor-Ceiling Concept for Clinical Assessment (i.e., Strengths and Limitations)
| Test | Technology | Strength | Limitation/Weakness | Floor | Ceiling |
| MMT | Nil - manual | No cost | Poor inter- and intra-reliability. Tester individual strength. | Uncommon in these client groups. | The majority of patients score a 4-5/5 utilizing MMT. Unable to manually detect strength deficits. |
| Visual Observations of Quality of Movement (QOM) and ROM During Functional Tasks (e.g., CMJ or hopping tasks). | Nil Video recording Smartphone Apps | Low/no cost | May be user-dependent for the quality of data obtained. | Individuals are unable to perform movement due to functional capacity, pathology or pain. | Visual QOM assessments are highly subjective and may not be able to detect sub-clinical deficits. |
| Jump Assessments | SmartphoneApplications Jump Mats | Low/no cost | Basic calculations of jump height via flight time. Do not capture QOM. | Require a base level of PF strength and Achilles tendon loading capacity to perform the test. | |
| Dynamometry | Push HHD ForceFrame (FFD) DynaMo (Compression, Tension and FPD) App Enabled for Feedback | Good intra-tester reliability and validity assessing the RFD (31, 32) and measures of peak force (32) of the hip musculature. Moderate to good validity of ankle and knee RFD measures. (32) | Unable to obtain data that reflects the function of the SSC. May need greater load capacity depending on the strength of the subject: DynaMo Plus – load capacity of 1,000N (100kg/220lbs) (compression). DynaMo Max – load capacity of 10,000N (1,000kg/2,200lbs). ForceFrame – load capacity of 2,500N (250kg/550lbs). | Minimum force threshold can be as low as 5 newtons. | When DynaMo Plus and DynaMo Max reach their limit. |
| ForceDecks – Jumps: CMJ, DJ, Hop | App-Enabled, Computer Enabled | An affordable price point, a high load ceiling and can assess dynamic and static movements. | Unable to isolate muscle groups for contributions to function (e.g., soleus vs. Gastrocnemius and hip muscles). | Minimum level of capacity required to perform tasks. |
Given the evolution of technology, evidence and best practices, the question is not so much, “Why utilize data-driven assessments in my clinical practice?” but “Which data-driven assessments best suit my clinical practice?”
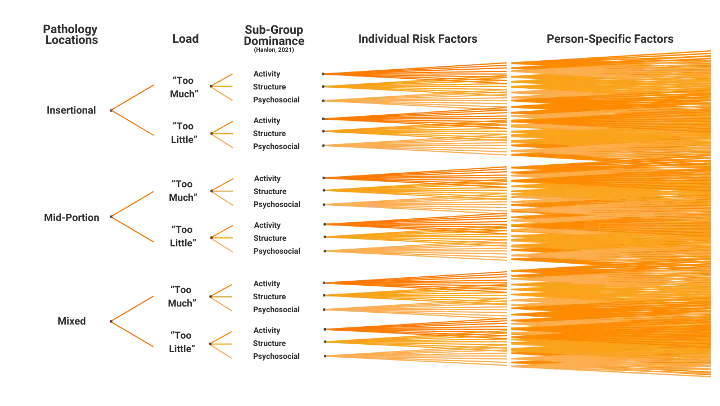
Developing Frameworks for Individualization
While there is widespread recognition that we need to individualize our management programs and therapeutic interventions, achieving efficiency and accuracy in our program formulation is built upon a foundation of consistency in our assessment frameworks.
…achieving efficiency and accuracy in program formulation is built upon a foundation of consistency in assessment frameworks.
Successful frameworks apply our understanding of pathology and address the various risk and individual factors that may contribute to its presentation. They also recognize the common functional deficits that may develop and determine where an individual may land on the pathology spectrum. Within clinical practice, we have non-specific elements of our frameworks, which include (but are not limited to) our ability to identify clients:
- Goals
- Health literacy and understanding of a pathology
- Motivators
- Barriers
Additionally, we then have the specific elements of our frameworks that allow us to:
- Understand a pathology, its various clinical presentations and treatment options.
- Assess and address a person’s current functional capacity and presenting functional deficits.
- Develop management plans that facilitate functional restoration and align with the client’s goals.
- Review, revise, progress and regress a rehabilitation program based on patient response.
Expanding upon our grasp of the importance of thorough assessment and management frameworks, the visual representation below can assist in choosing the most suitable equipment and testing techniques based on your patient’s current capacity or rehabilitation stage. This will enhance your clinical assessments.
The question isn’t so much, “Should I use technology in my clinical assessments?” It is more so “Which technology should I use in my clinical assessments?”
Understanding the clinical utility of technology, the metrics it assesses and how it may influence your management plans, coupled with the client demographics you see and the goal activities you are often programming to return your clients to, will help answer this question.
In addition to data-driven assessments providing an avenue for better-informed clinical decision-making regarding exercise selection and loading decisions, the utilization of technology within clinical practice provides simple and effective ways to address numerous elements considered integral to exercise treatment adherence. These include: (30)
- Facilitating the linking of the client’s goals to our therapeutic goals.
- Providing real-time, tangible data to help educate clients and facilitate “buy-in” to a prescribed movement program.
- Developing micro-goals to create “manageable goals.”
- Longitudinally tracking changes in metrics.
In summary, the recommendation of data-driven approaches is not to replace existing validated methods of assessment, such as VISA-A, VISA-A (sedentary) and TENDINS-A; instead, it aims to enable a more proactive approach to management through more informed clinical decisions and facilitating the overcoming of common barriers that exist in our clients’ rehabilitation engagement.
If you would like to know more about the value of implementing technology into your organization, please reach out.
References
- Tarantino D, Mottola R, Resta G, et al. Achilles Tendinopathy Pathogenesis and Management: A Narrative Review. International Journal of Environmental Research and Public Health. 2023;20(17):6681. doi:https://doi.org/10.3390/ijerph20176681
- Winnicki K, Ochała-Kłos A, Rutowicz B, Pękala PA, Tomaszewski KA. Functional anatomy, histology and biomechanics of the human Achilles tendon — A comprehensive review. Annals of Anatomy - Anatomischer Anzeiger. 2020;229:151461. doi:https://doi.org/10.1016/j.aanat.2020.151461
- Fukutani A, Sawatsky A, Leonard T, Walter H. Contribution of the Achilles tendon to force potentiation in a stretch–shortening cycle. The Journal of Experimental Biology. 2019;222(14):jeb204032. doi:https://doi.org/10.1242/jeb.204032
- Faude O, Donath L. Editorial: Neuromuscular Performance During Lifespan: Assessment Methods and Exercise Interventions. Frontiers in Physiology. 2019;10:1348. doi:https://doi.org/10.3389/fphys.2019.01348
- Quarmby A, Mönnig J, Mugele H, et al. Biomechanics and lower limb function are altered in athletes and runners with achilles tendinopathy compared with healthy controls: A systematic review. Frontiers in Sports and Active Living. 2023;4. doi:https://doi.org/10.3389/fspor.2022.1012471
- Malliaras P. Physiotherapy management of Achilles tendinopathy. Journal of Physiotherapy. 2022;68(4)221-237. doi:https://doi.org/10.1016/j.jphys.2022.09.010
- Corrigan P, Hornsby S, Pohlig RT, Willy RW, Cortes DH, Grävare Silbernagel K. Tendon loading in runners with Achilles tendinopathy: relations to pain, structure, and function during return‐to‐sport. Scandinavian Journal of Medicine & Science in Sports. Published online April 30, 2022. doi:https://doi.org/10.1111/sms.14178
- Chen W, Cloosterman KLA, Bierma-Zeinstra SMA, van Middelkoop M, de Vos RJ. Epidemiology of insertional and midportion Achilles tendinopathy in runners: A prospective cohort study. Journal of Sport and Health Science. 2023;13(2). doi:https://doi.org/10.1016/j.jshs.2023.03.007
- McAuliffe S, Tabuena A, McCreesh K, et al. Altered Strength Profile in Achilles Tendinopathy: A Systematic Review and Meta-Analysis. Journal of Athletic Training. 2019;54(8):889-900. doi:https://doi.org/10.4085/1062-6050-43-18
- Wang YH, Zhou HH, Nie Z, Cui S. Prevalence of Achilles tendinopathy in physical exercise: A systematic review and meta-analysis. Sports Medicine and Health Science. 2022;4(3):152-159. doi:https://doi.org/10.1016/j.smhs.2022.03.003
- Bovend’Eerdt TJ, Botell RE, Wade DT. Writing SMART rehabilitation goals and achieving goal attainment scaling: a practical guide. Clinical Rehabilitation. 2009;23(4):352-361. doi:https://doi.org/10.1177/0269215508101741
- Habets B, van den Broek AG, Huisstede BMA, Backx FJG, van Cingel REH. Return to Sport in Athletes with Midportion Achilles Tendinopathy: A Qualitative Systematic Review Regarding Definitions and Criteria. Sports Medicine. 2017;48(3):705-723. doi:https://doi.org/10.1007/s40279-017-0833-9
- Grävare Silbernagel K, Crossley KM. A Proposed Return-to-Sport Program for Patients with Midportion Achilles Tendinopathy: Rationale and Implementation. Journal of Orthopaedic & Sports Physical Therapy. 2015;45(11):876-886. doi:https://doi.org/10.2519/jospt.2015.5885
- McAuliffe S, Tabuena A, McCreesh K, et al. Altered Strength Profile in Achilles Tendinopathy: A Systematic Review and Meta-Analysis. Journal of Athletic Training. 2019;54(8):889-900. doi:https://doi.org/10.4085/1062-6050-43-18
- Abdelsattar M, Konrad A, Tilp M. Relationship between Achilles Tendon Stiffness and Ground Contact Time during Drop Jumps. Journal of Sports Science and Medicine. 2018;17(2):223-228. PMID: 29769823; PMCID: PMC5950739
- Silbernagel KG, Gustavsson A, Thomeé R, Karlsson J. Evaluation of lower leg function in patients with Achilles tendinopathy. Knee Surgery, Sports Traumatology, Arthroscopy. 2006;14(11):1207-1217. doi:http://dx.doi.org/10.1007/s00167-006-0150-6
- Gravare Silbernagel K, Thomee R, Eriksson BI, Karlsson J, Khan K. Full symptomatic recovery does not ensure full recovery of muscle-tendon function in patients with Achilles tendinopathy. British Journal of Sports Medicine. 2007;41(4):276-280. doi:https://doi.org/10.1136/bjsm.2006.033464
- Silbernagel KG, Hanlon S, Sprague A. Current Clinical Concepts: Conservative Management of Achilles Tendinopathy. Journal of Athletic Training. 2020;55(5):438-447. doi:https://doi.org/10.4085/1062-6050-356-19
- Murphy M, Travers M, Gibson W, et al. Rate of Improvement of Pain and Function in Mid-Portion Achilles Tendinopathy with Loading Protocols: A Systematic Review and Longitudinal Meta-Analysis. Sports Medicine. 2018;48(8):1875-1891. doi:https://doi.org/10.1007/s40279-018-0932-2
- de Jonge S, van den Berg C, de Vos RJ, et al. Incidence of midportion Achilles tendinopathy in the general population. British Journal of Sports Medicine. 2011;45(13):1026-1028. doi:https://doi.org/10.1136/bjsports-2011-090342
- Habets B, Smits HW, Backx FJG, van Cingel REH, Huisstede BMA. Hip muscle strength is decreased in middle-aged recreational male athletes with midportion Achilles tendinopathy: A cross-sectional study. Physical Therapy in Sport. 2017;25:55-61. doi:https://doi.org/10.1016/j.ptsp.2016.09.008
- J Jackson SM, Cheng MS, Smith AR, Kolber MJ. Intrarater reliability of hand held dynamometry in measuring lower extremity isometric strength using a portable stabilization device. Musculoskeletal Science and Practice. 2017;27:137-141. doi:https://doi.org/10.1016/j.math.2016.07.010
- Shimizu Y, Tsutsui S, Katoh M. Examination and reliability of measuring muscle strength of ankle plantar flexion with knee extended. Journal of Physical Therapy Science. 2023;35(9):619-623. doi:https://doi.org/10.1589/jpts.35.619
- Norris R, Cook JL, Gaida JE, Maddox T, Raju J, O’Neill S. The VISA-A (sedentary) should be used for sedentary patients with Achilles tendinopathy: a modified version of the VISA-A developed and evaluated in accordance with the COSMIN checklist. British Journal of Sports Medicine. 2023;57(20):1311-1316. doi:https://doi.org/ 10.1136/bjsports-2022-105547
- Lui Q. Data Analyses with Ceiling/Floor data. cran.r-project.org. Accessed 2018. Available from: https://cran.r-project.org/web/packages/DACF/vignettes/DACF-vignette.html
- O’Neill S. A Biomechanical Approach to Achilles Tendinopathy Management [thesis]. University of Leicester; 2016. Available from: https://figshare.le.ac.uk/articles/thesis/A_biomechanical_approach_to_Achilles_tendinopathy_management/10209797. Submitted for the degree of Doctor of Philosophy.
- Phillips R, Hilton C, Fernando L, Farlie M, Morrissey D, Malliaras P. Behaviour change and rehabilitation adherence in adults with tendinopathy: a scoping review. Disability and Rehabilitation. Published online February 29, 2024:1-13. doi:https://doi.org/10.1080/09638288.2024.2320832
- van der Vlist AC, Breda SJ, Oei EHG, Verhaar JAN, de Vos RJ. Clinical risk factors for Achilles tendinopathy: a systematic review. British Journal of Sports Medicine. 2019;53(21):1352-1361. doi:https://doi.org/10.1136/bjsports-2018-099991
- Franettovich Smith MM, Honeywill C, Wyndow N, Crossley KM, Creaby MW. Neuromotor control of gluteal muscles in runners with achilles tendinopathy. Medicine & Science in Sports & Exercise. 2014;46(3):594-599. doi:https://doi.org/10.1249/mss.0000000000000133
- Collado-Mateo D, Lavín-Pérez AM, Peñacoba C, et al. Key Factors Associated with Adherence to Physical Exercise in Patients with Chronic Diseases and Older Adults: An Umbrella Review. International Journal of Environmental Research and Public Health. 2021;18(4):2023. doi:https://doi.org/10.3390/ijerph18042023.
- Ishøi L, Hölmich P, Thorborg K. MEASURES OF HIP MUSCLE STRENGTH AND RATE OF FORCE DEVELOPMENT USING A FIXATED HANDHELD DYNAMOMETER: INTRA-TESTER INTRA-DAY RELIABILITY OF A CLINICAL SET-UP. International Journal of Sports Physical Therapy. 2019;14(5):715-723. doi:https://doi.org/10.26603/ijspt20190715
- Mentiplay BF, Perraton LG, Bower KJ, et al. Assessment of Lower Limb Muscle Strength and Power Using Hand-Held and Fixed Dynamometry: A Reliability and Validity Study. Haddad JM, ed. PLoS One. 2015;10(10):e0140822. doi:https://doi.org/10.1371/journal.pone.0140822
- Lorimer AV, Hume PA. Achilles Tendon Injury Risk Factors Associated with Running. Sports Medicine. 2014;44(10):1459-1472. doi:https://doi.org/10.1007/s40279-014-0209-3
- Demangeot Y, Whiteley R, Gremeaux V, Degache F. The load borne by the Achilles tendon during exercise: A systematic review of normative values. Scandinavian Journal of Medicine & Science in Sports. 2022;33(2):110-126. doi:https://doi.org/10.1111/sms.14242
- Murphy MC, Newsham-West R, Cook J, et al. TENDINopathy Severity assessment – Achilles (TENDINS-A): Development and Content Validity assessment of a new Patient-Reported Outcome Measure for Achilles Tendinopathy. Journal of Orthopaedic & Sports Physical Therapy. 2023;(11):1-16. doi:https://doi.org/10.2519/jospt.2023.11964
- Davis PR, McKay MJ, Baldwin JN, Burns J, Pareyson D, Rose KJ. Repeatability, consistency, and accuracy of hand-held dynamometry with and without fixation for measuring ankle plantarflexion strength in healthy adolescents and adults. Muscle & Nerve. 2017;56(5):896-900. doi:https://doi.org/10.1002/mus.25576