Hip Replacement Rehabilitation: Tracking recovery with HumanTrak
Available in:
EN
Case Background
Joan, a 72-year-old, maintained her daily physical activity through evening walks and gardening. However, over time, worsening osteoarthritis (OA) in her right hip made these activities increasingly painful, ultimately limiting her physical activity levels.
After months of on-and-off physiotherapy, her functional status began to decline, leaving her unable to walk or garden without pain. After a referral for imaging and further medical workup, her orthopedic surgeon recommended a total hip arthroplasty (THA). Joan understood her mobility would be limited during recovery, but she remained focused on returning to the meaningful activities she enjoyed most.
Rehabilitation Overview
Joan’s physiotherapist scheduled a visit one week prior to her surgery to gather pre-operative baseline data on her movement using HumanTrak. The following assessments were used to assess her pre-surgery movement:
| Assessment | Metric | Importance | Initial Evaluation Data |
| Quiet Stand |
Center of mass 95% ellipse area
Anteroposterior center of mass excursion | Measures balance and favoring of one side over the other |  |
| Seated Hip Internal and External Rotation | Range of motion (ROM) | Measures joint mobility required to perform daily tasks | 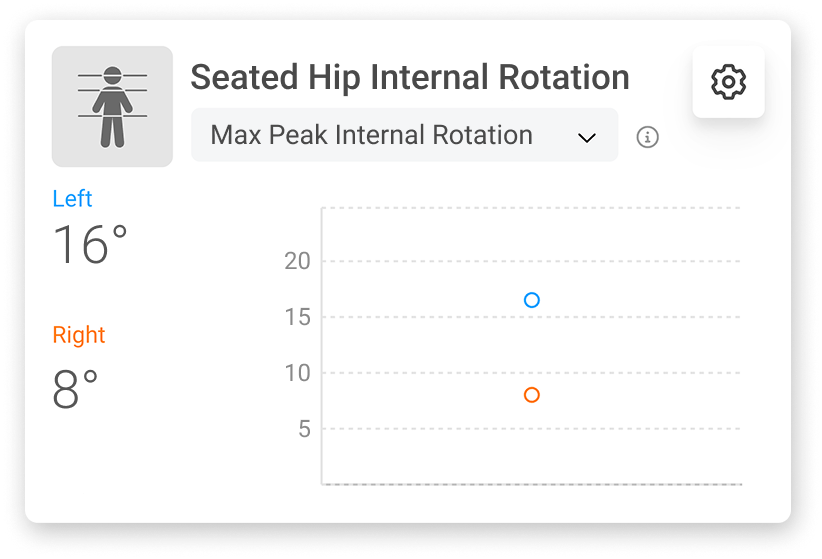 |
| Squat | Hip flexion and pelvic tilt ROM | Measures mobility and coordination required to perform daily tasks |  |
12-Month Rehabilitation Program
Following a successful right hip replacement, Joan began a 12-month rehabilitation program focused on restoring mobility and functional capacity to support her return to daily activity (Lowe et al., 2009). Her program included weekly appointments with her physiotherapist, where her progress was continually assessed. After each session, her data was uploaded to VALD Hub for her physiotherapist to review.
…Joan began a 12-month rehabilitation program focused on restoring mobility and functional capacity to support her return to daily activity.
With her physiotherapist’s guidance, Joan downloaded the MoveHealth app to complete and record her home exercise programs (HEPs), review educational materials about her condition and track key HumanTrak metrics. She could also view her previous patient-reported outcome measure (PROM) scores, allowing her to see how her pain, stiffness and daily function changed throughout her recovery.

Patient using the MoveHealth app to view her scheduled tasks.
Weeks 1-3
Core and hip strengthening exercises in a seated and prone position formed the foundation of Joan’s early rehabilitation. These low-load movements helped restore strength and stability without placing unnecessary stress on the hip.
Week 6-12
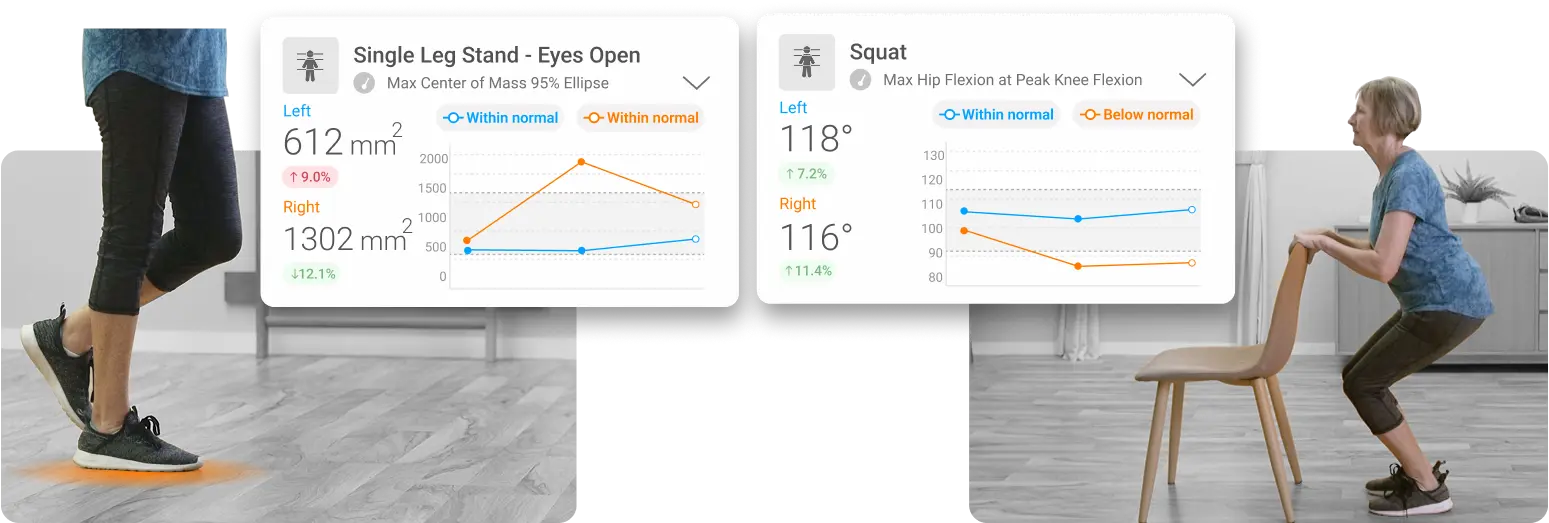
At six weeks, the single leg stand test assessed Joan’s balance and hip abductor control. The results helped her physiotherapist identify side-to-side differences in hip stability and adjust her walking progression accordingly.

Single leg stand and squat tests performed using HumanTrak.
Balancing on her right leg was challenging, but HumanTrak’s real-time visualizations helped optimize both her balance testing and training, targeting improvements in hip strength and control.
From six weeks post-surgery, Joan’s physiotherapist gradually introduced more advanced variations of HumanTrak’s squat test into her weekly sessions. The test served as a practical measure of hip and knee extensor strength. Initially, Joan performed shallow squats within a limited range to minimize hip flexion and adhere to post-surgical precautions.
Weeks 12+
By 12 weeks post-surgery, Joan’s squat depth had significantly improved. Bilateral hip flexion measures were becoming more symmetrical, and her total volume of tolerable squats increased substantially.

VALD Hub tile highlighting overall improvements in squat depth and hip flexion asymmetry.
Improvements in her squat ability and balance began translating to functional, meaningful activity as Joan returned to evening walks and more consistent HEP participation, guided by center of mass and ROM metrics.
Joan’s balance and squat measures improved, guided by her HEP participation and advice from her physiotherapist.
Over the course of her rehabilitation, Joan and her physiotherapist used HumanTrak to assess and guide progressions in balance, joint mobility and overall functional capacity. The staged progression of her rehabilitation is outlined below:
| Timeframe | Assessment | Measurement | Importance | Comparison |
| 3-6 Weeks | Standing posture (5 seconds) |
Peak spine and pelvic lateral tilt
Absolute motion of the center of mass | Indicates balance and favoring of one side over the other | Longitudinal (including baseline) |
| 6-9 Weeks | Standing posture (5 seconds) |
Peak spine and pelvic lateral tilt
Absolute motion of the center of mass | Indicates balance and favoring of one side over the other | Longitudinal (including baseline) |
| Squat (ensuring the hip does not flex past 90°) |
Hip flexion
Successful performance (Y/N) | Indicates control of hip muscles | Longitudinal | |
| Single leg stand |
Peak pelvic lateral tilt
Successful performance (Y/N) | Indicates control of hip muscles and balance | Contralateral | |
| 9-12 Weeks | Standing posture (5 seconds) |
Peak spine and pelvic lateral tilt
Absolute motion of the center of mass | Indicates balance and favoring of one side over the other | Longitudinal (including baseline) |
| Single leg stand | Peak pelvic lateral tilt | Indicates control of hip muscles and balance | Longitudinal and with contralateral | |
| Squat repetition test | Hip flexion at peak knee flexion, repetition number | Proxy measure for hip strength-endurance and functional mobility | Longitudinal | |
|
12 Weeks- 1 Year | Seated hip internal and external rotation | Hip internal and external rotation ROM | Indicates flexibility | Baseline |
| Squat repetition test | Hip flexion at peak knee flexion, repetition number | Proxy measure for hip strength-endurance and functional mobility | Baseline |
Solutions and Advantages
HumanTrak provides consistent and reliable analysis of kinematic tasks beyond visual observation. By assessing and quantifying variables such as pelvic anterior or lateral tilt, practitioners can more accurately track the effectiveness of their interventions on qualities like hip strength and control, often cited as fall risk factors (Porto et al., 2019).
With consistent tracking over time, Joan’s weekly standing posture and single leg stand tests provided directly comparable metrics, giving her physiotherapist confidence in monitoring true changes over time.
…standing posture and single leg stand tests provided directly comparable metrics, giving her physiotherapist confidence in monitoring true changes over time.
Based on her progress, her physiotherapist incorporated lateral hip strengthening exercises into her HEP, which contributed to improvements in pelvic lateral tilt during the single leg stand test. The consistent use of reliable technologies, such as HumanTrak, gave them both confidence that the improvements reflected true increases in hip abductor strength rather than variations in measurement technique.
Patient performing banded hip abduction from her prescribed HEP in the MoveHealth app.
Using MoveHealth, Joan’s physiotherapist could easily share her progress after each session and monitor her HEP participation. The app’s clear visuals and longitudinal comparisons allowed Joan to track her improvements over time, without the need for manually generated reports.
Using PROMs to Guide Decision-Making
Hip OA is a chronic condition where symptoms may fluctuate – sometimes worsening, improving or remaining stable for long periods. Flare-ups are common and often prompt medical review, though they do not always indicate structural decline.
For many patients, including Joan, the most disruptive symptoms include pain, stiffness, reduced participation in daily activities, disturbed sleep and overall decreased quality of life. Because these experiences are subjective, PROMs are crucial for quantifying symptom impact and guiding management.
Within MoveHealth, Joan’s physiotherapist selected from several available PROMs, primarily focusing on the Copenhagen Hip and Groin Outcome Score (HAGOS) to monitor her pain, stiffness and functional limitations throughout rehabilitation. While other PROMs, such as the Western and McMaster Universities Arthritis Index (WOMAC), are also accessible, the HAGOS provided a clear and consistent measure of Joan’s progress, helping track symptom changes and guide ongoing care decisions.
…HAGOS provided a clear and consistent measure of Joan’s progress, helping track symptom changes and guide ongoing care decisions.
One-Year Follow-Up
Each week, Joan could see her progress visualized on-screen through HumanTrak, reinforcing that her rehabilitation was on track. The objective metrics gave both Joan and her physiotherapist confidence to safely reintroduce her evening walks as strength and control improved.
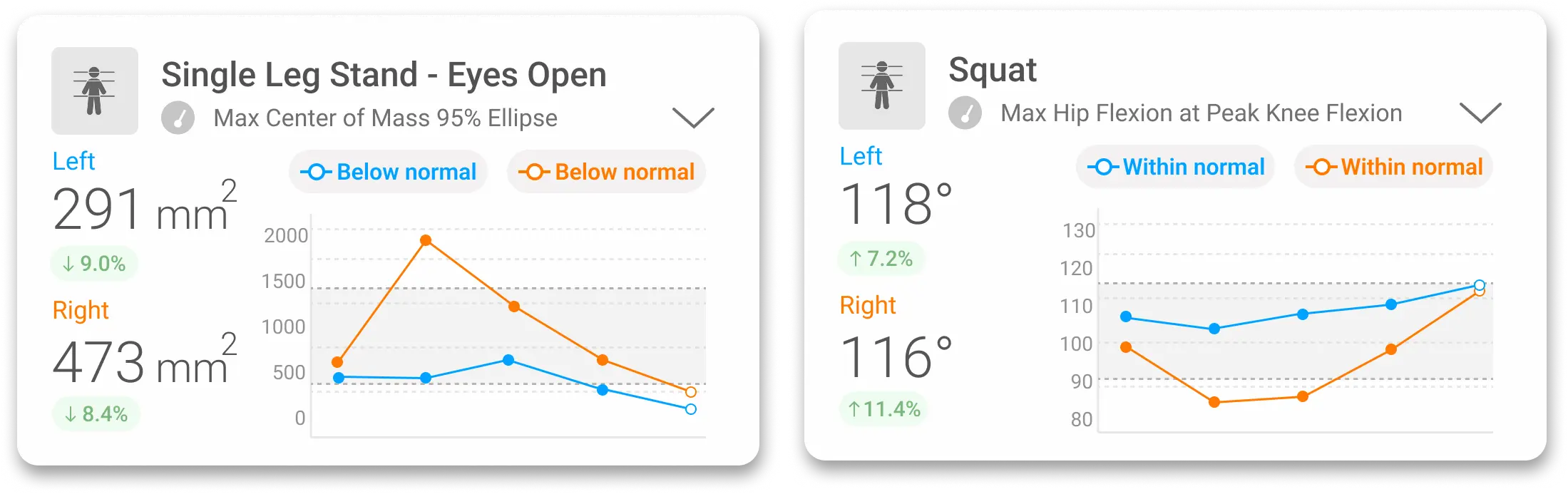
Single leg stance and squat test results visualized in VALD Hub, confirming good recovery one year post-surgery.
After one year, HumanTrak data confirmed full recovery from her hip replacement, with mobility and control metrics in the squat and single leg stand assessments surpassing her pre-surgery function. Joan attended her one-year orthopedic review, where her objective improvements were clearly documented and supported by consistent longitudinal data.
If you would like to learn more about how HumanTrak can support hip replacement rehabilitation, track recovery progress and inform clinical decision-making, get in touch with our team.
References
- Lowe, C. J. M., Barker, K. L., Dewey, M. E., & Sackley, C. M. (2009). Effectiveness of physiotherapy exercise following hip arthroplasty for osteoarthritis: A systematic review of clinical trials. BMC Musculoskeletal Disorders, 10(1), 98. https://doi.org/10.1186/1471-2474-10-98
- Porto, J. M., Júnior, R. C. F., Bocarde, L., Fernandes, J. A., Marques, N. R., Rodrigues, N. C., & de Abreu, D. C. C. (2019). Contribution of hip abductor–adductor muscles on static and dynamic balance of community-dwelling older adults. Aging Clinical and Experimental Research, 31(5), 621–627. https://doi.org/10.1007/s40520-018-1025-7
