Neurological Rehab: Bringing objectivity to practice
Available in:
EN
The following article was written for clinicians working in neurological rehabilitation who are looking to integrate objective strength assessment into practice. Developed with contributions from Michelle Kahn, PhD, it highlights practical applications of DynaMo for assessing and improving walking function in neurologic populations.
Force production is a fundamental component of effective walking. Therefore, quantifying force production is necessary for effective physiotherapy care in populations struggling with ambulation (Dorsch et al., 2016).
Populations that suffer from neurologic impairments, such as incomplete spinal cord injuries (SCI) or stroke, have critical thresholds of force production required for effective walking, whether that be assisted or unassisted. This makes traditional measurement approaches in rehabilitation, such as manual muscle testing (MMT), fall short due to their lack of sensitivity, reliability and generalizability to functional outcomes.
Objective measurement technology is reshaping neurological assessment. Handheld dynamometers (HHDs) such as DynaMo allow clinicians to quantify strength with accuracy and consistency, supporting more targeted management strategies for walking.
Objective measurement technology is reshaping neurological assessment …[allowing] clinicians to quantify strength with accuracy and consistency…

Common applications of HHDs seen in neurological populations.
Technology plays a central role in assessing and treating adults with mobility and walking limitations. Its sensitivity allows for greater detection of improvements or decline, guiding future intervention strategies in populations such as stroke, traumatic brain injury, cerebral palsy, multiple sclerosis, SCI and other neurological conditions (Williams et al., 2013; Shortland, 2009; Jørgensen et al., 2017).
Rehabilitation programs are designed to help patients achieve meaningful improvements in walking ability. Goals typically focus on greater independence, speed, endurance, strength or functional appearance. To achieve these outcomes, physiotherapists can use dynamometry (e.g., DynaMo) to deliver precise strength assessments, supporting the following:
- Individualized treatment planning
- Objective tracking of strength changes
- Targeted interventions supporting gait and functional outcomes
Muscle Strength Assessment
Patients struggle with walking from a range of etiologies. Therefore, physical evaluations require a comprehensive assessment of various walking-related impairments:
- Lower-limb muscle strength and power
- Muscle length
- Muscle tone and spasticity
- Balance
Quantifying weakness is essential to neurological physiotherapy to highlight key deficits, track progress over time and inform targeted interventions to improve walking function.
Quantifying weakness is essential to neurological physiotherapy to highlight key deficits, track progress over time and inform targeted interventions…
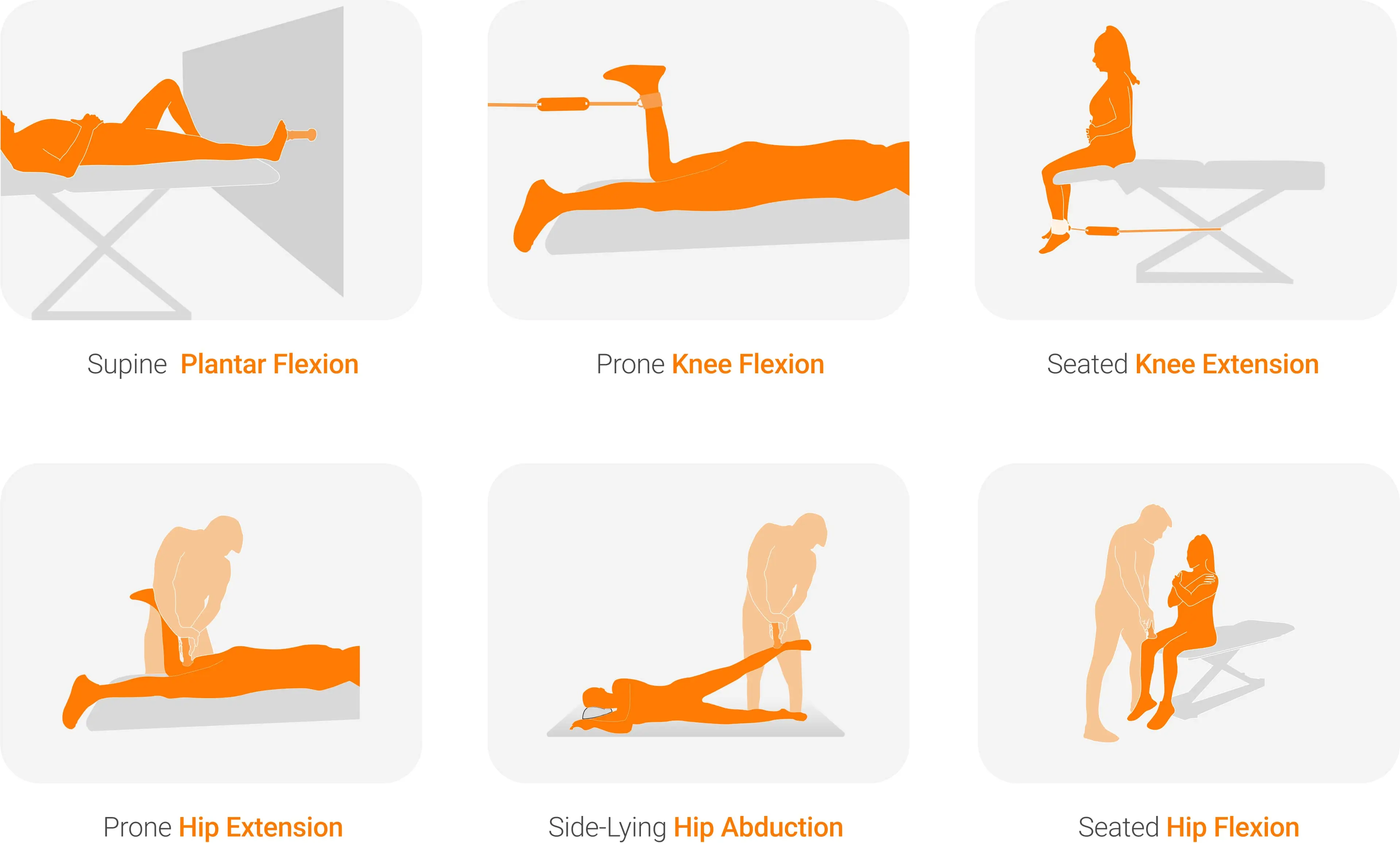
Lower extremity strength assessment options. Find these and more protocols on VALD’s Knowledge Base.
Assessment Methods
Typical clinical strength assessments, such as MMTs, are basic and often lack accuracy (Bohannon, 2005). Using a six-point ordinal scale, clinicians using MMTs are often unable to detect strength differences of up to 30% between limbs (MacAvoy & Green, 2007).
HHDs, however, provide a clinically feasible and objective measure of strength, with strong clinimetric properties due to their objectivity, reliability and comparability to various standards or benchmarks, such as Norms (Stark et al., 2011; Bonhof-Jansen et al., 2022).
HHDs, however, provide a clinically feasible and objective measure of strength…due to their objectivity, reliability and comparability to various standards or benchmarks, such as Norms.
Assessing muscle strength for walking efficiency dives deeper than basic muscle strength (Dorsch et al., 2018; Neptune et al., 2008). Isometric rate of force development (RFD) is a helpful surrogate measure for lower extremity power, a key determinant of walking ability (Aagaard et al., 2002). This is particularly important for three primary movers in walking – the ankle plantar flexors, hip flexors and hip extensors (Liu et al., 2006).

Enhancing Clinical Practice with Objective Tools
Measuring maximal and rate-dependent force qualities like peak force and RFD enables clinicians working in neurological rehabilitation to monitor attributes specific to functional tasks such as walking.
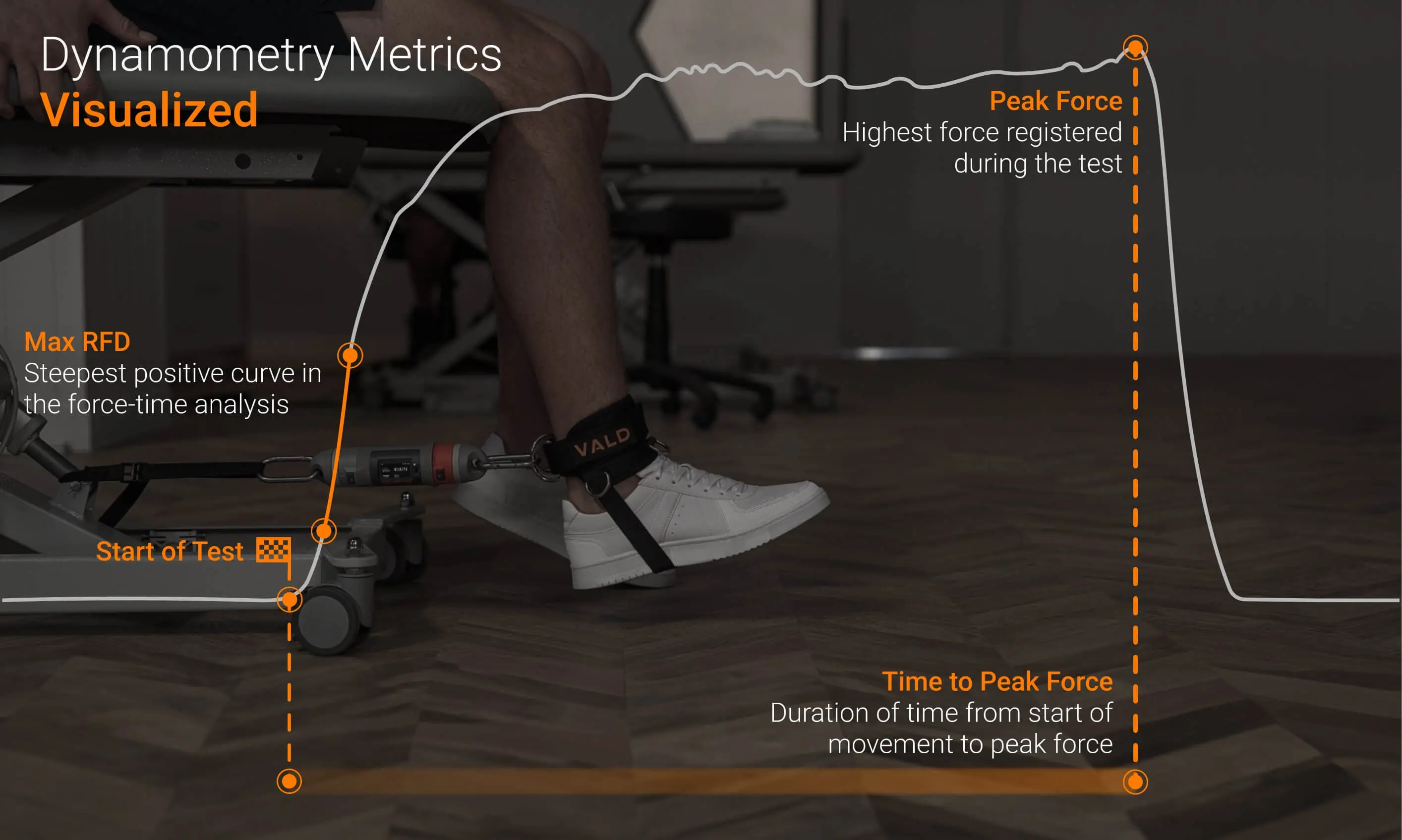
Visual depiction of common metrics used in dynamometry, such as peak force, RFD and time to peak force.
With these capabilities, clinicians can accurately quantify the neuromuscular qualities that enable or negatively impact walking performance.
…clinicians can accurately quantify the neuromuscular qualities that enable or negatively impact walking performance.
Integrating Objective Assessment in the Clinic
Test battery features can be used to create customized testing protocols. This allows clinicians treating patients with walking impairments to streamline testing by position order, reducing testing time and the burden on patients whose mobility may be limited.
For example, clinicians working with neurologic populations often use test batteries to capture the strength of muscle actions important for walking, such as:
- Knee flexion and extension
- Hip flexion, extension and abduction
- Ankle plantar flexion and dorsiflexion
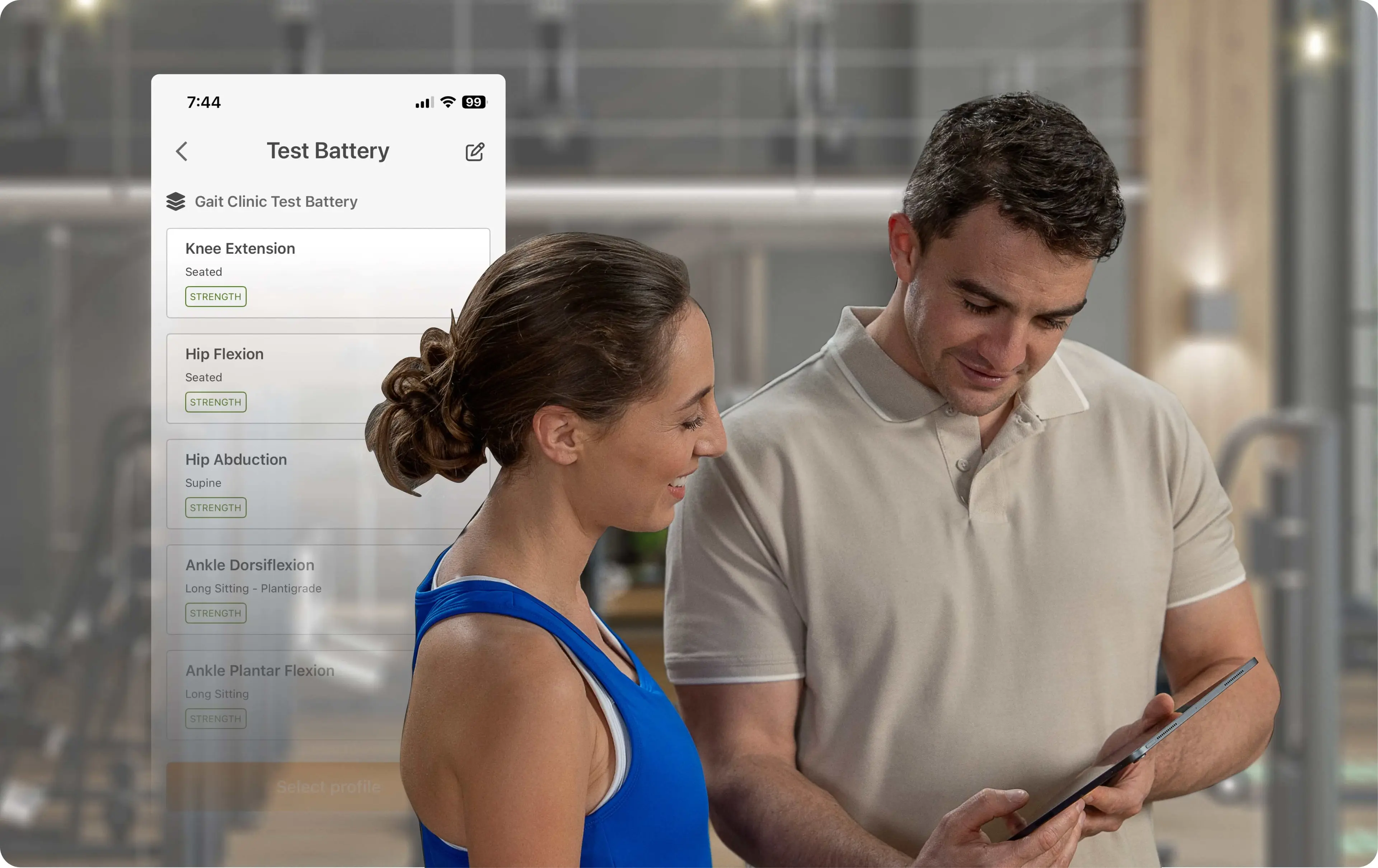
Clinician and patient discussing a test battery performed in the clinic.
DynaMo is sensitive and reliable enough to pick up very low and very high muscle force production, ensuring consistent measurement across a wide range of patients.
DynaMo is sensitive and reliable enough to pick up very low and very high muscle force production, ensuring consistent measurement across a wide range of patients. Results are simple to interpret, directly comparable to prior sessions and highlight specific muscles to target in strength programs.
Serial assessments displayed in the DynaMo app and VALD Hub quantify progress, evaluate intervention effectiveness and provide valuable longitudinal insights – particularly for monitoring potential decline in progressive neurological conditions.
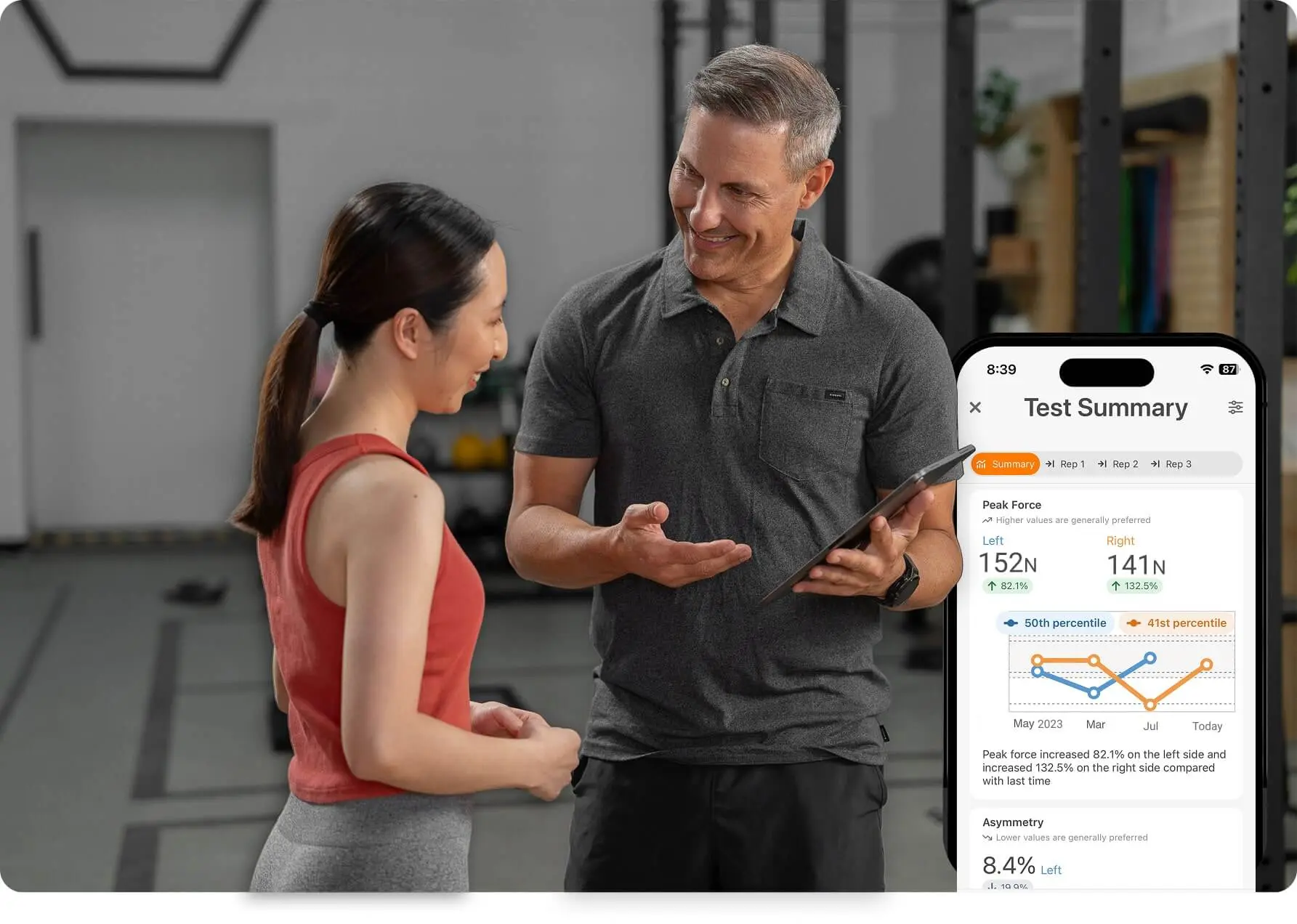
Testing summary showing longitudinal monitoring with in-app Norms.
Patient Benefits of Objective Muscle Strength Data
Neurological rehabilitation is a gradual process, with meaningful improvements often occurring over extended periods. Traditional clinical assessments (e.g., MMT) lack sensitivity to subtle changes and can be difficult to interpret in functional terms. In contrast, objective data provides clear evidence of progress to the patient and contributes to the following benefits:
- Greater confidence in the assessment process and the clinicians overseeing their care, supported by objective, professional reporting
- Accurate, numerical data to guide clinical decisions and ensure continuity between therapy providers
- Clear visualization of progress through graphs, percentage changes and serial comparisons, which helps patients understand the benefits of their rehabilitation and stay motivated
- Specific, targeted feedback on areas to improve, including asymmetry measures for patients with hemiplegia to support progression toward normal movement
Testing for Optimized Return to Function
Objective strength assessment has become essential to neurological rehabilitation, providing clinicians and patients with clear, reliable data to guide progress and improve walking outcomes. Tools like DynaMo enable clinicians to measure changes in muscle function, track recovery over time and make data-informed decisions that enhance both care quality and patient confidence.
If you are a clinician in neurological rehabilitation seeking greater objectivity in strength assessment, contact us to learn how DynaMo Plus can support your decision-making and improve patient outcomes.
References
- Dorsch, S., Ada, L., & Canning, C. G. (2016). Lower limb strength is significantly impaired in all muscle groups in ambulatory people with chronic stroke: A cross-sectional study. Archives of Physical Medicine and Rehabilitation, 97(4), 522–527. https://linkinghub.elsevier.com/retrieve/pii/S0003999315014264
- Williams, G. P., Schache, A. G., & Morris, M. E. (2013). Mobility after traumatic brain injury: Relationships with ankle joint power generation and motor skill level. The Journal of Head Trauma Rehabilitation, 28(5), 371–378. https://doi.org/10.1097/htr.0b013e31824a1d40
- Shortland, A. (2009). Muscle deficits in cerebral palsy and early loss of mobility: can we learn something from our elders? Developmental Medicine & Child Neurology, 51, 59–63. https://doi.org/10.1111/j.1469-8749.2009.03434.x
- Jørgensen, M.-L. K., Dalgas, U., Wens, I., & Hvid, L. (2017). Muscle strength and power in persons with multiple sclerosis–A systematic review and meta-analysis. Journal of the Neurological Sciences, 376, 225–241. https://linkinghub.elsevier.com/retrieve/pii/S0022510X17301910
- Bohannon, R. W. (2005). Manual muscle testing: does it meet the standards of an adequate screening test? Clinical Rehabilitation, 19(6), 662–667. https://doi.org/10.1191/0269215505cr873oa
- MacAvoy, M. C., & Green, D. P. (2007). Critical reappraisal of medical research council muscle testing for elbow flexion. The Journal of Hand Surgery, 32(2), 149–153. https://doi.org/10.1016/j.jhsa.2006.10.020
- Stark, T., Walker, B., Phillips, J. K., Fejer, R., & Beck, R. (2011). Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: a systematic review. PM&R, 3(5), 472–479. https://doi.org/10.1016/j.pmrj.2010.10.025
- Bonhof-Jansen, E. D. J., van Ham, A., Kroon, G. J., Winter, R. W., & Brink, S. M. (2022). Validity and reliability of a portable handheld dynamometer compared to a fixed isokinetic dynamometer to assess forearm torque strength. Hand Surgery and Rehabilitation, 42(2), 147–153. https://doi.org/10.1016/j.hansur.2022.12.003
- Dorsch, S., Ada, L., & Alloggia, D. (2018). Progressive resistance training increases strength after stroke but this may not carry over to activity: a systematic review. Journal of Physiotherapy, 64(2), 84–90. https://doi.org/10.1016/j.jphys.2018.02.012
- Neptune, R. R., Sasaki, K., & Kautz, S. A. (2008). The effect of walking speed on muscle function and mechanical energetics. Gait & Posture, 28(1), 135–143. https://doi.org/10.1016/j.gaitpost.2007.11.004
- Aagaard, P., Simonsen, E. B., Andersen, J. L., Magnusson, P., & Dyhre-Poulsen, P. (2002). Increased rate of force development and neural drive of human skeletal muscle following resistance training. Journal of Applied Physiology, 93(4), 1318–1326. https://doi.org/10.1152/japplphysiol.00283.2002
- Liu, M. Q., Anderson, F. C., Pandy, M. G., & Delp, S. L. (2006). Muscles that support the body also modulate forward progression during walking. Journal of Biomechanics, 39(14), 2623–2630. https://doi.org/10.1016/j.jbiomech.2005.08.017
