Post-Surgical Shoulder Rehab for a Professional Baseball Pitcher
Available in:
EN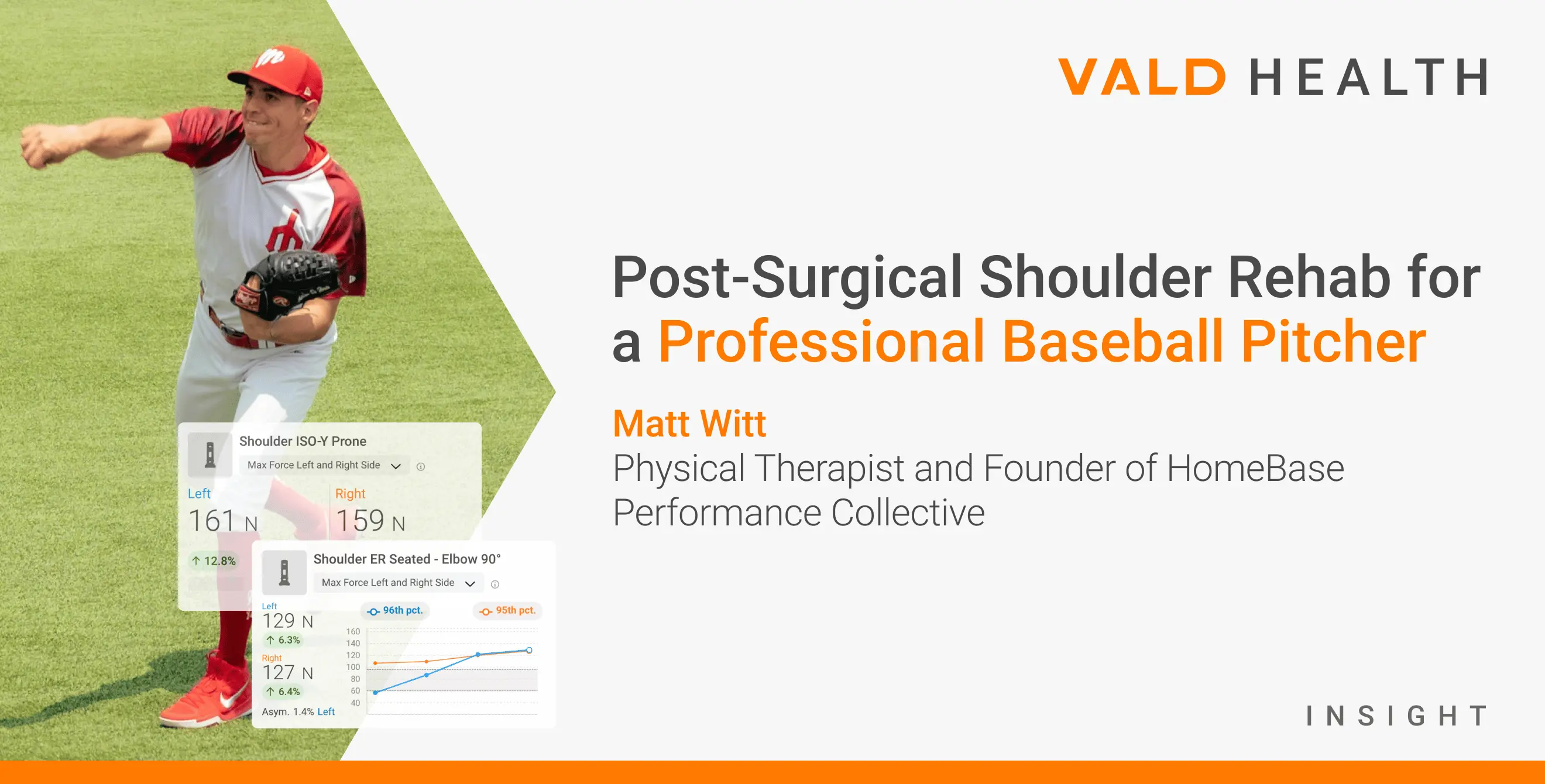
About the Author
Matt Witt, PT, DPT, MS, CSCS, is a physical therapist and founder of HomeBase Performance Collective, based in Central Kentucky. He has experience in outpatient orthopedics and professional sports, having worked as a physical therapist for the New York Mets and Cleveland Guardians.
He also brings industry expertise in healthcare and performance technology, having served as a business development manager.
This case study follows the shoulder rehab journey of Sammy, a professional baseball pitcher, as he progresses through a structured, five-phase return-to-throwing program.
It forms part of the Practitioner’s Guide to Shoulders and highlights how objective data from VALD’s DynaMo, ForceFrame and ForceDecks was used to track, test and adjust rehab at every stage – supporting a safe and successful return to play.
Phase 1
Early Post-Operative Care (Weeks 0-4)
Key Goals:
- Protect surgical repair
- Avoid active movement of the shoulder
- Initiate passive range of motion (PROM) in protected ranges (no external rotation [ER])
Sammy’s shoulder was immobilized for four weeks post-surgery. During this time, only passive motion within the scapular plane was allowed. The medical staff was able to measure and progress the passive range of the shoulder using the DynaMo strapped to Sammy’s upper arm.
The medical staff was able to measure and progress the passive range of the shoulder using the DynaMo…
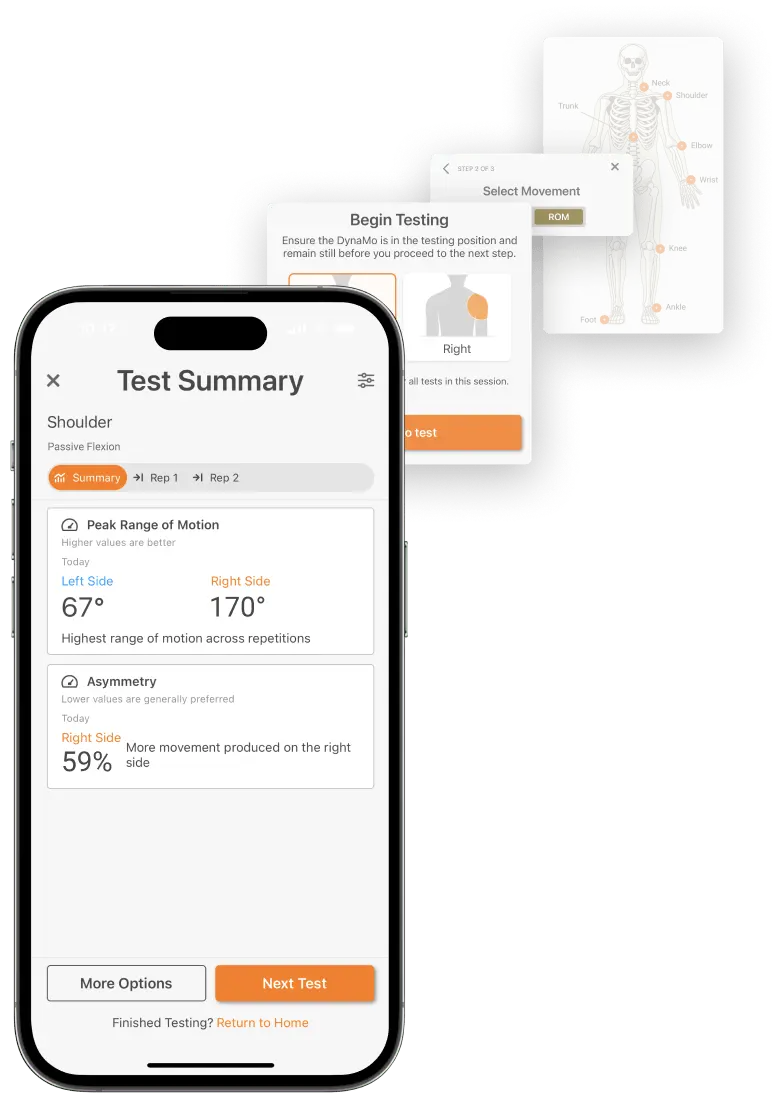
PROM measured using DynaMo, with in-app results highlighting asymmetry between the injured and uninjured sides to help guide ongoing rehab progression.
Phase 2
Initiate Low-Intensity Muscle Activation (Weeks 5-8)
Key Goals:
- Progress active range of motion (AROM) in flexion and abduction
- Initiate PROM and active assisted range of motion (AAROM) of ER at increasing angles of shoulder abduction
- Introduce submaximal isometrics in neutral ranges
AAROM was initiated at week five. Traditional AAROM progressions were applied with progress indicated through DynaMo measurements weekly.
Additionally, kinetic chain and scapular strengthening exercise progressions were initiated. Once full AAROM of flexion and abduction was achieved, AROM exercises and rotator cuff strengthening exercises began.
Once full AAROM of flexion and abduction was achieved, AROM exercises and rotator cuff strengthening exercises began.
Phase 3
Reconditioning (Weeks 8-16)
Key Goals:
- Increase and maintain shoulder ROM
- Initiate progressive shoulder strengthening (peak force)
- Introduce progressive submaximal testing cadence
Shoulder flexion and abduction were maintained while ER in increasing angles of shoulder abduction was gradually restored. Progress was continuously measured using DynaMo.
Once fully restored, weekly ROM checks were completed to gauge tolerance to exercise progression. An isometric rotator cuff strengthening program within protected ranges was initiated at week eight. The medical staff first used the DynaMo to measure Sammy’s subjective output with flexion, abduction, ER and internal rotation (IR) in the neutral position.
The medical staff first used the DynaMo to measure Sammy’s subjective output… [before initiating] a long-duration, low-intensity isometric training program on the ForceFrame.
Once the subjective output was objectified, a long-duration, low-intensity isometric training program was initiated on the ForceFrame.
| “Give me 4/10 effort” | |||
|---|---|---|---|
| Flexion at Mid-ROM | Abduction at Mid-ROM | IR at 0 | ER at 0 |
| 60N | |||
| 50N | 55N | 45N | |
In conjunction with traditional isotonic rotator cuff and kinetic chain exercises, the low-intensity, long-duration isometric program was progressed. Gradually, intensity was increased and duration shortened to a scheme promoting max strength.
Additionally, the amount of shoulder abduction with ER and IR training was progressed from neutral to a 90/90 (layback) position, all being performed on the ForceFrame.
Tolerance to the isometric strength training program could be tracked through ForceFrame’s “time in zone” and “variance” metrics.
Tolerance to the isometric strength training program could be tracked through ForceFrame’s “time in zone” and “variance” metrics. Using the feedback from those metrics, modifications to intensity and duration could be made to ensure the desired stimulus was achieved.

ER and IR isometric training in a 90/90 position using ForceFrame, with longitudinal tracking of average impulse, time in zone and variance to guide adjustments to training intensity and duration.
A submaximal testing cadence was created to begin estimating max force production while conditioning the shoulder to increase force production.
Submaximal Testing Cadence (Subjective % Effort)
| Weeks | Shoulder ER:IR (at Supine 90) | Shoulder ER:IR (at 90/90) |
|---|---|---|
| Week 13 | 75% | 50% |
| Week 14 | 75% | 50% |
| Week 15 | 90% | 75% |
| Week 16 | 90% | 75% |
Objective measurement of the submaximal tests combined with Sammy’s subjective report gave the staff insight into the progress of Sammy’s shoulder strength. Using pre-injury data, the medical staff could benchmark his progress and set realistic goals for Sammy’s max force capacity.
Phase 4
Sport-Specific Readiness (Weeks 17-23)
Key Goals:
- Initiate upper body and throwing plyometric progression
- Progress shoulder rate of force development (RFD) training
- Perform maximal shoulder strength testing
At week 17, training was shifted to prep the shoulder for the high-speed demands of throwing. Sammy’s ForceFrame training program included high-intensity (>85%) and short-duration (<5) reps.
Upper body plyometrics and throwing plyometric exercises were initiated and progressed through the phase. Max testing of shoulder ER:IR was performed and used to inform the medical staff if shoulder strength was adequate to begin a throwing program.
Max testing of shoulder ER:IR was performed and used to inform the medical staff if shoulder strength was adequate to begin a throwing program.
Athletic Shoulder (ASH) testing was also initiated in this phase, as the staff was interested in the RFD value from performance on the ForceDecks.
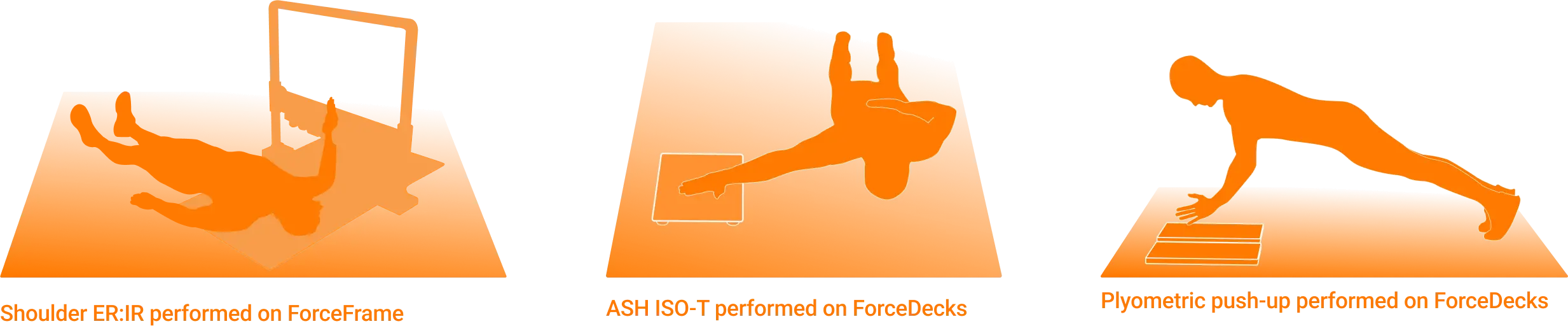
Examples of upper body plyometric and maximal isometric strength tests used during the sport-specific readiness phase to assess both force and RFD.
Clearance Testing Cadence
| Weeks | Shoulder ER:IR (Supine Elbow at 90) | Shoulder ER:IR (Supine at 90/90) | ASH Test (Y) |
|---|---|---|---|
| Week 17 | 100% | 90% | Not Tested |
| Week 18 | Not Tested | 100% | 50% |
| Week 19 | Not Tested | Not Tested | 75% |
| Week 20 | 100% | Not Tested | 75% |
| Week 21 | Not Tested | Not Tested | 90% |
| Week 22 | Not Tested | 100% | 90% |
| Week 23 | 100% | Not Tested | 100% |
Phase 5
Throwing Program Progression (Weeks 24-48)
Key Goals:
- Progress throwing load to meet sports demand
- Begin testing cadence for routine
- Maintain strength and ROM
A summary of Sammy’s objective shoulder strength testing demonstrated readiness to begin his throwing program at week 24.
| 100% Strength Testing Results | Shoulder ER:IR (Supine at 90) | Shoulder ER:IR (at 90/90) | ASH Test Y (Peak/RFD) |
|---|---|---|---|
| Results | 200/230N | 200/230N | 170N/443N/s |
| Goal (75th percentile of population) | >210/224N | >150/180N | >165N/>500N/s |
*ASH Test Y RFD normative value not reported.
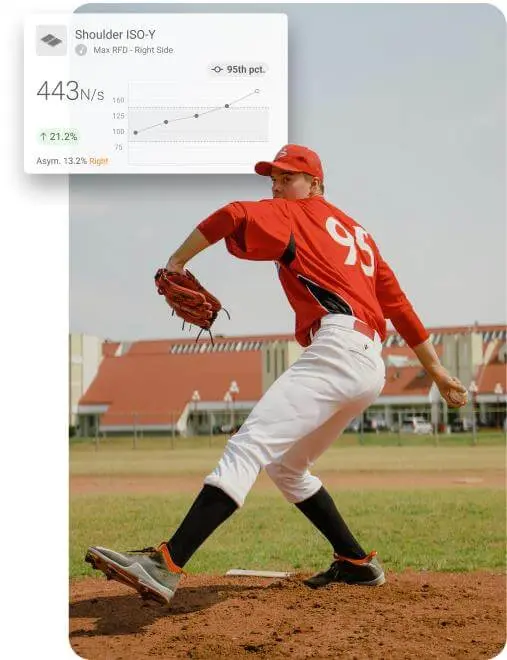
ASH Test (Y) results displayed in VALD Hub help guide return-to-throw decisions.
Routine monitoring of shoulder ER:IR strength was collected biweekly. Modifications to the throwing program and deloads were built in as acute changes in shoulder strength were observed.
Modifications to the throwing program and deloads were built in as acute changes in shoulder strength were observed.
Weekly ROM checks were also conducted, as acute changes in ROM could indicate poor tolerance to the throwing program. Sammy progressed through the throwing program and was able to successfully return to games.
If you are looking to enhance your approach to shoulder rehab with objective testing, force monitoring and return-to-throwing protocols, explore our Practitioner’s Guide to Shoulders. To learn more or to integrate VALD technology into your practice, reach out to our team.
