Transforming Healthcare: technology for all abilities and all ages
Available in:
EN
Exercise Healthcare Australia (EHA) was founded to bring elite level exercise services to people of all ages and abilities.
EHA’s founder Mitchell Vautin witnessed the impact of exercise on people with chronic disease, disability, and pain and realised these individuals needed the same level of care and support that professional athletes receive. Thus, EHA was created to provide the best possible care, attention, and support to achieve the best possible outcomes. EHA’s team is committed to helping those who need it with the latest evidence-based practice in the best possible environment.
Here's what their clients have to say about the service.
In their pursuit of this mission, in late 2021 EHA introduced ForceDecks into their practice, then subsequently DynaMo, following its launch in 2022. Now almost 18 months on from integrating VALD technology into their organisation, EHA are within the top DynaMo users across the globe. Recently, Mitchell was asked to present at the Exercise and Sports Science Australia Conference (ESSA Annual Conference) on the impacts that objective measurement technology has had for his clients, staff and his business.
After his presentation we spoke with Mitchell to find out a little more and to share some of the key points he presented.
Why did EHA implement VALD technology?
EHA brought VALD into our clinical practice following its successful implementation at Athletes Authority. The thought process at this time was “why should only athletes be using this technology?” Our clientele – people with chronic disease, disability or frailty, along with elderly and paediatrics alike ought to be assessed with the same, if not greater level of care in order to achieve the best possible outcomes.
Our clientele – people with chronic disease, disability or frailty, along with elderly and paediatrics alike ought to be assessed with the same, if not greater level of care [as elite athletes] in order to achieve the best possible outcomes.

We started with ForceDecks, which transformed our way of assessing lower limb strength, biomechanics and balance. When VALD released the DynaMo, following the success of using the ForceDecks we knew that we had to have it.
The DynaMo has now allowed us to effectively assess strength and joint range of motion for all of our patients. Our goal for every client is to do a minimum of at least one upper and lower body objective strength measurement using DynaMo or ForceDecks (or both).
Our goal for every client is to do a minimum of at least one upper and lower body objective strength measurement using DynaMo or ForceDecks (or both).
What benefits have you seen since implementing VALD technology?
Implementing VALD technology has had some great benefits for our patients and us – the health professionals providing care. For our team of Clinical Exercise Physiologists, we have been able to communicate our depth of understanding of the patient following their initial assessment more effectively.
We believe that a lot of people go to see their GP and their physiotherapist to know what is wrong with them – they want to receive a diagnosis. As Exercise Physiologists (whilst we cannot exactly provide a diagnosis), through the use of the objective data collected with VALD’s technologies, we are able to provide a comprehensive hypothesis. This hypothesis is based on our knowledge that if we are able to identify then address the deficits measured with the testing with an appropriate exercise program, the patient will be able to move closer towards their goal – whatever that may be.
For our team of Clinical Exercise Physiologists, we have been able to communicate our depth of understanding of the patient following their initial assessment more effectively … through the use of the objective data collected with VALD’s technologies, we are able to provide a comprehensive hypothesis.
We have also noticed a lot more buy-in from our patients. It could be deflating for patients who work hard for weeks on end without being able to see any changes in their body, but being able to see their numbers has completely changed this. Now, being able to physically see and quantify exactly how much they are improving every six weeks at their re-assessment has been instrumental in demonstrating that their hard work is paying off.
We have also noticed a lot more buy in from our patients … being able to physically see and quantify exactly how much they are improving every six weeks at their re-assessment has been instrumental in demonstrating that their hard work is paying off.
Can you tell us about any specific cases where the data you collected has had a meaningful impact?
Case Study 1: 65-Year-Old Male with Parkinson’s Disease, Multifocal Motor Neuropathy.
This patient exhibits a right foot drop, ambulates with a 4 - wheeled - walker and is currently undergoing chemotherapy and immunoglobin therapy. The Insurance Provider recommended reducing from twice weekly exercise physiology services to fortnightly services – essentially a 75 % reduction in therapy sessions.
Our traditional outcome measures initially showed progress, but over time they became insensitive. For example, his 30 second sit to stand had increased from 5 repetitions at his initial assessment to 14 reps, but then had stagnated for a period of around 4 months despite ongoing rehabilitation. The nature of the 30 second sit to stand simply did not provide a meaningful enough measure of strength or rate of force development, which can be much more impactful to someone’s life.
On the other hand, when we assessed his Isometric Mid-Thigh Pull (IMTP) in the same four month period, we were able to see that – despite his stagnation in the 30 second sit to stand test – his maximal strength and rate of force development had increased significantly.
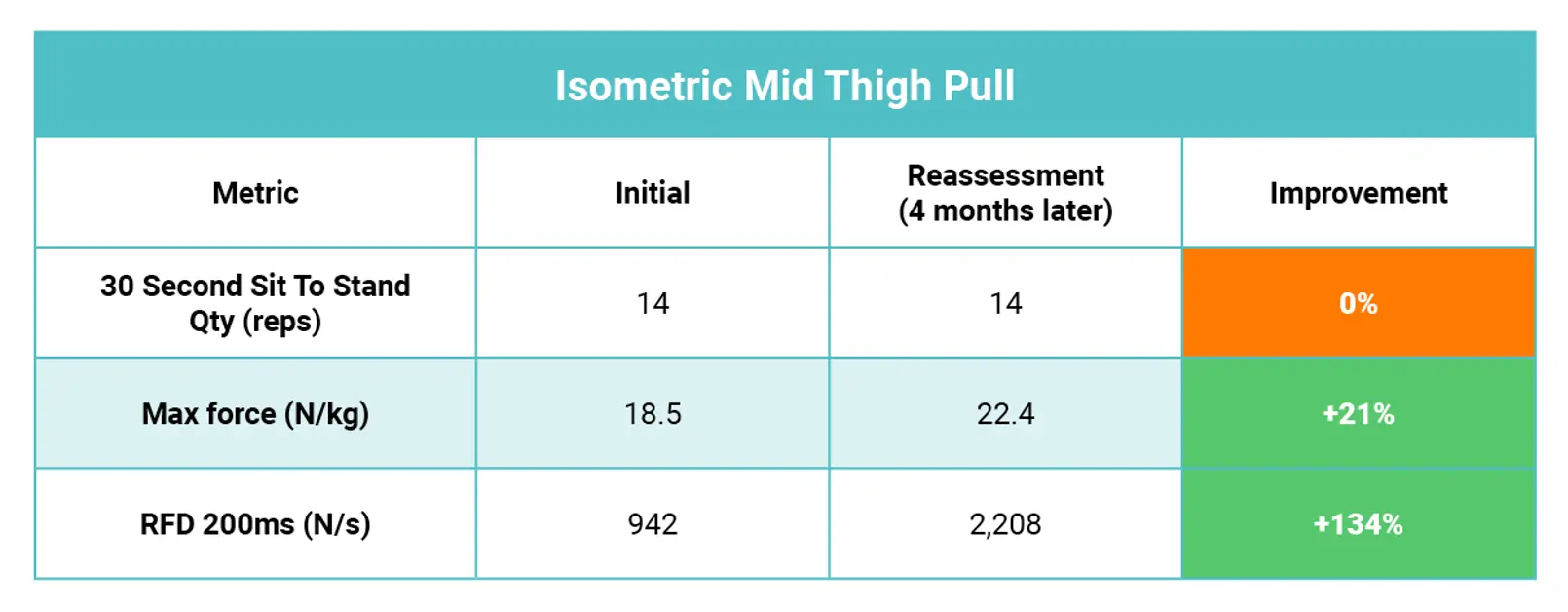
This data was able to help successfully reverse the decision, enabling the client to continue to twice weekly therapy with EHA, as we were able to demonstrate – with objective data – that they were making real, meaningful progress.
Case Study 2: 31-Year-Old Male, Severed Peroneal Nerve with Foot Drop.
This patient’s insurer required a return-to-work clearance, but the patient reported that he was still feeling unsteady – particularly standing on his right side – and did not feel ready to return to work as a result. A traditional test of single leg balance for time showed he could maintain balance for an above average result of more than 45 seconds on each side. There was a conflict in what the patient was reporting and what our balance test showed.
The issue was that his medical insurance was based on his functional capacity and getting him to a point where he could effectively return to work. Our challenge was that we needed to be able to show that what he was feeling was real and that we could help him improve.
ForceDecks did just that – in a similar single leg balance test (but this time, measured with precise data), it showed significant variances in objective measures that traditional testing was incapable of measuring. The patient’s ForceDecks results are shown in the table below.
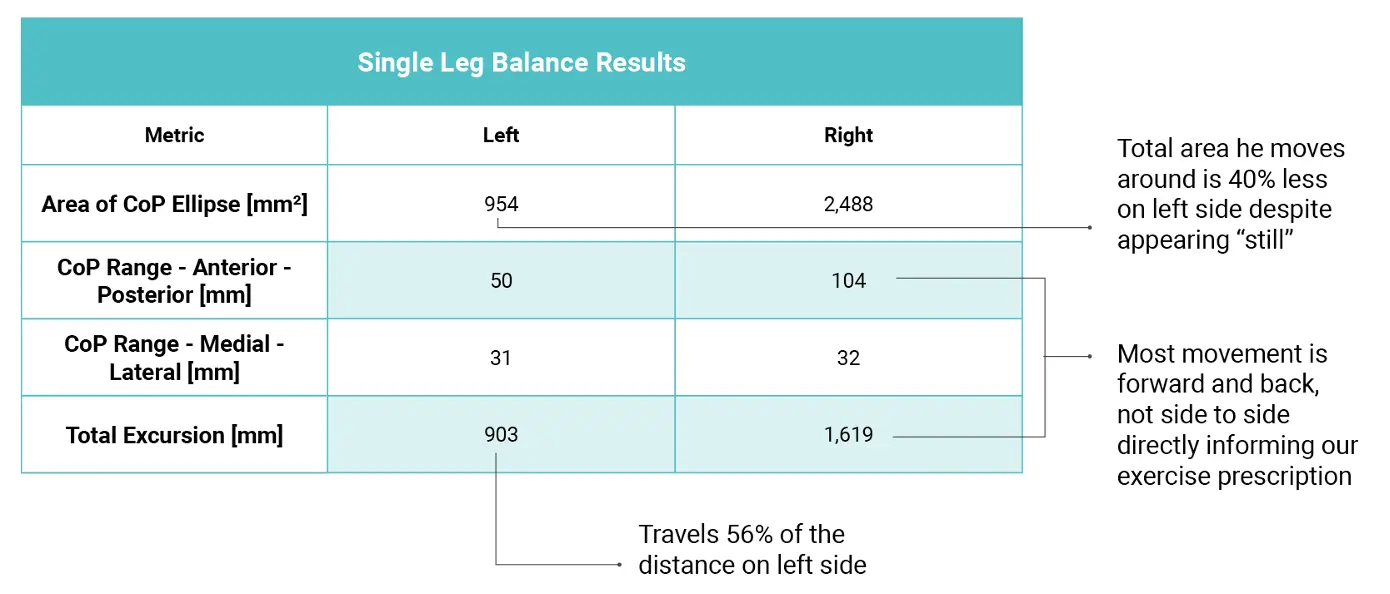
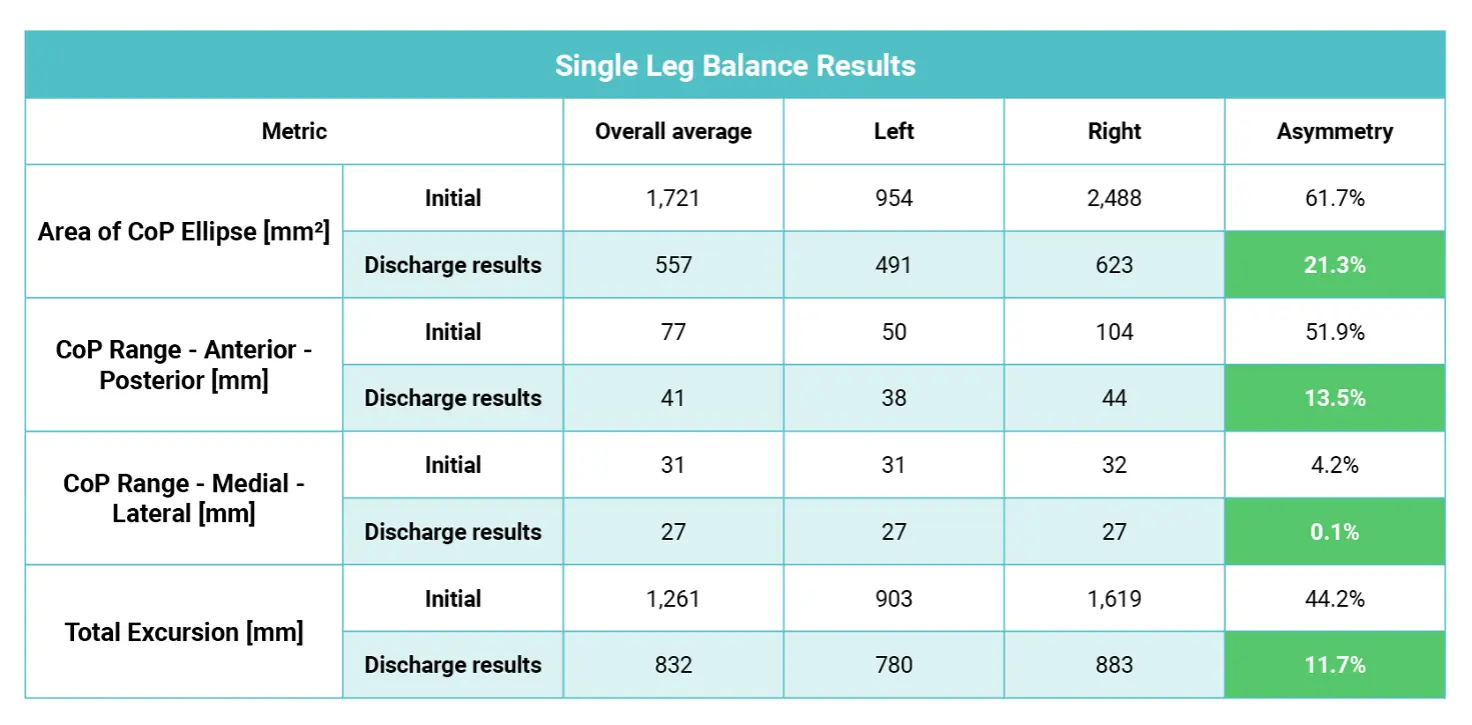
These findings provided the justification his insurer needed to allow him to access EHA’s rehabilitation services, measure his ongoing progress, and then return to work safely once his objective results were at a point where they were significantly improved and matched his subjective reports.
Case Study 3: 68-Year-Old Female, Right Adductor Tendinopathy, Multiple Comorbidities
To help with her condition, this patient had been prescribed a series of adductor strengthening exercises by another health provider. The patient reported that they hadn’t received any objective strength testing to inform the program that they had received. After approximately 6 weeks of consistently performing these exercises, the patient was frustrated at her lack of progress and decided to seek a second opinion in the hopes of getting back into exercise again.
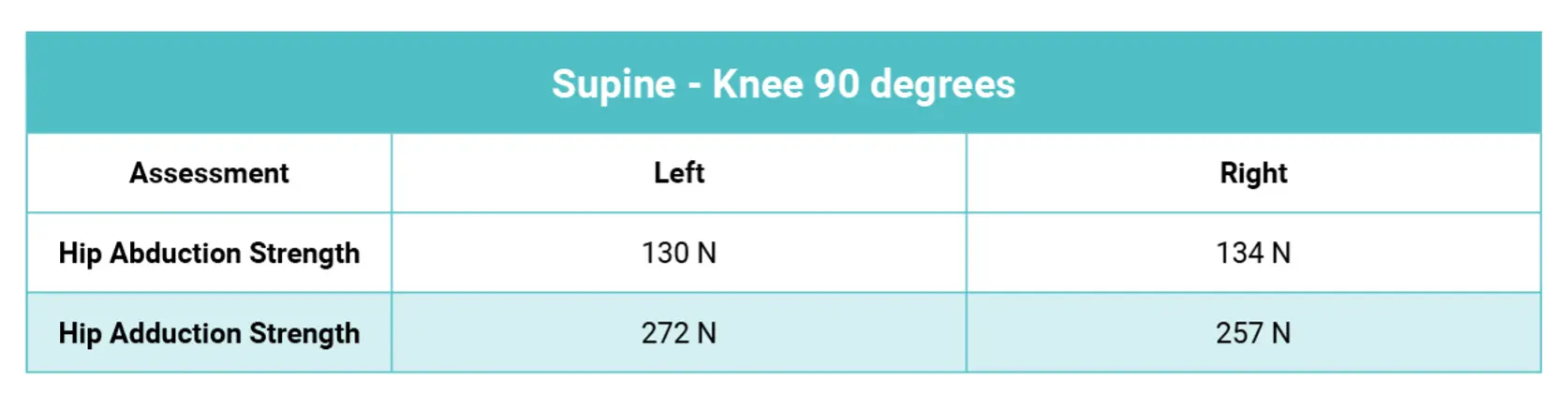
During our initial assessment, we tested her strength using DynaMo. We saw that, in fact, it was her abductors that were lacking strength, not her symptomatic adductors (results shown in the table below). Accordingly, we changed her program to prescribe abduction-based exercises, and in turn she was able to return to daily activities without pain as well as returning to exercise classes.

What impact has implementing VALD technology had on your staff?
The Exercise Physiologists certainly love using the technology and a lot now say they couldn’t see themselves doing their jobs without it. When interviewing new staff, we often get feedback that having this technology is another attractive reason to join our team.
The Exercise Physiologists certainly love using the technology and a lot now say they couldn’t see themselves doing their jobs without it.
Has there been a return on investment (ROI)?
Yes – a very significant ROI from our perspective. Using just one of the cases discussed earlier, we were able to continue twice-weekly services that would otherwise have been reduced to fortnightly. Put simply, it helped the client have access to approximately 70 additional consultations over the course of the year. This example alone would be enough for us to see a positive ROI, but we have been seeing many examples like this across our team of 17 exercise physiologists.
This example alone would be enough for us to see a positive ROI, but we have been seeing many examples like this across our team of 17 exercise physiologists.
In addition to introducing VALD technology we changed a number of other processes in our business over the last 12 months. We have seen that – despite working in low socioeconomic areas with people who don’t know what an exercise physiologist is or does – we have been able to double our average number of sessions per patient from 6 to just above 12.
Now, while not every patient necessarily needs more sessions, we do believe that if we can help someone for the first 3 months of their treatment – getting them through the hardest part of changing a behaviour – that is when we can see a life-changing impact.
Do you have any key learnings from implementing VALD technology, or were there any barriers you needed to overcome?
A few things:
- Don’t be overwhelmed by the amount of information you can receive from the technology. Siphon out what is most important to you and the individual that is in front of you and use that.
- Be careful of analysis paralysis – especially when considering there are over 200 metrics that are captured by ForceDecks.
- Remember: you care about the data more than most of the patients you work with. It becomes most powerful when you can connect objective data with something that is meaningful to your patients, like their activities of daily living that they may be struggling with and how improving strength or movement will make them easier.
Any other comments or thoughts about your experience?
If you’re working in health with the goal of improving someone’s range of motion, balance, strength or power: if you are not measuring, you are guessing. Without the insights provided by using objective measurement technology, you simply cannot provide the same service to a client, no matter how much experience you have. I could not see EHA doing it any other way.
If you’re working in health with the goal of improving someone’s range of motion, balance, strength or power: If you are not measuring, you are guessing … I could not see EHA doing it any other way.
The team at VALD are exceptional – nothing is ever too hard or out of reach. It’s amazing to see that the technology (despite how great it already is) is constantly evolving and improving. It is great to work with an organisation that listens to feedback and often many of the changes we have seen directly reflect the feedback we have provided.
If you would like to know more about how to integrate VALD’s human measurement technology into your organisation to help with the engagement of your clients, please reach out here.
