What will telehealth’s future look like post-COVID-19?
Available in:
EN
If you’re asking if telehealth will continue in a post-COVID-19 world, you’re asking the wrong question.
Rather, the question we should be asking is, what consultation option is the best for my client?
It’s not as simple as ‘to telehealth or not to telehealth’, but instead a question of how telehealth can be sustainably integrated into our models of service delivery. The best consultation option for your client will depend on your client’s clinical presentation and preferences, as well as your expert clinical judgement. Realistically, this may see practitioners transitioning between several options as we see technology increasingly accepted and embraced in clinical practice.

TeleHealth in a Pre-COVID World
In a pre-COVID world, uptake of telehealth was low, and historically primarily used to overcome the barrier of distance (Cottrell & Russell 2020). In the midst of COVID-19 restrictions, allied health service providers were forced to pivot to telehealth appointments, which provided a quick and effective solution to continuing care while maintaining physical distancing. Despite being a steep learning curve for some and similarly for their clients, as a necessity, it was embraced. Since then restrictions have begun to ease in some locations, and as we move forward into a post-COVID world, we have an opportunity to think strategically about how an integrated model of care looks like for both practitioners and clients.
A traditional model of healthcare involves face-to-face assessment and treatment, typically combined with a home exercise program.
“This traditional model is costly to the health system, has a high client burden with respect to travel, and gives the practitioner limited visibility of progress, or opportunities to intervene, between face-to-face consults.”
In comparison, a tech-integrated model, which could incorporate a range of face-to-face, telehealth and remote monitoring of home programs could result in reduced burden, much higher visibility and more consistent monitoring, and at a lower cost to the system.
Delivery option one: face-to-face consult
Face-to-face consults can be indicated for a number of reasons. Initial assessments and reassessments may require or include hands-on measures that can’t be administered, or are not optimal over telehealth. Hands-on treatment may be required as part of the clients’ treatment plan; where safety is a concern if the client is unsupervised or alone during assessment or treatment; or simply when the client preference is to receive treatment face-to-face.
Delivery option two: telehealth consult
Real-time telehealth consults could be used as an adjunct to face-to-face appointments, or in isolation. Telehealth consults may be indicated for: assessment and reassessments with integration or adaptation of outcome measures appropriate for telehealth delivery; delivery of treatment particularly when focused on advice and education and exercise prescription; where physical distancing is still required or distance is a barrier to healthcare access (this may include access to specialist practitioners which otherwise would not be possible); and client preference.
Delivery option three: home exercise program amendment
Technology can give practitioners greater visibility of client progress between consults than ever before. Exercise prescription platforms such as TeleHab allow practitioners to remotely monitor their clients progress with their home exercise programs through exercise diaries, client-recorded videos and collection of outcome measures such as self-reported pain and ratings of perceived exertion (RPE).
“Telehealth is not simply about physical distancing and the convenience of not travelling to the clinic.”
With greater visibility via remote exercise monitoring, there is more opportunity for health professionals to intervene sooner and to modify a clients’ program without requiring a real-time consult via face-to-face or telehealth. Remote monitoring and real-time program modifications are also likely to improve adherence to home exercise programs, which is reportedly as low as 30% (Essery et al 2017) despite the high level of evidence to support the role of exercise in rehabilitation (O’Keefe et al 2017).
Not all clients need face-to-face consults, and some need more than others – How do we choose?
Let’s take a client with chronic Achilles tendinopathy as an example which is being managed over time by a health professional.
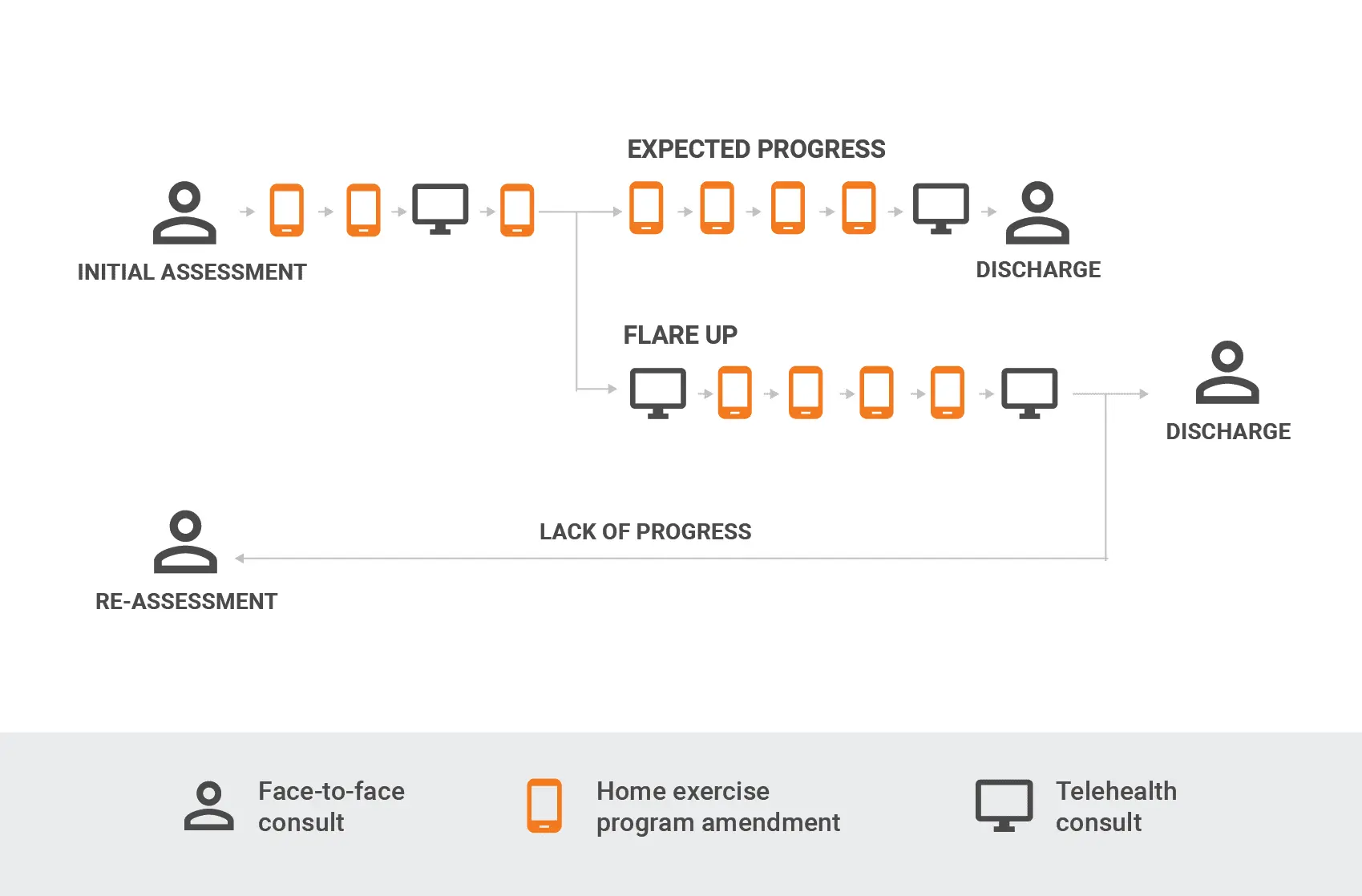
An initial consult could take place via a face-to-face consult including a client interview, baseline assessment and initial treatment which may include advice and education, passive therapy and prescription of a home exercise program. Interim follow-up consults may include modifying sets, reps, and load of calf raise programs; and exercises addressing other contributing factors via remote monitoring, with real-time consults via face-to-face or telehealth.
Painful flare-ups are common in Achilles tendinopathy, and in some cases cannot be managed by the client independently. In this instance, a telehealth consult would be appropriate to provide advice and education on appropriate running load management and exercise program changes beyond simple progressions to support the client to self-manage. This may be followed again by a combination of home exercise program modifications and telehealth consults.
If the client is not progressing as would be expected, a face-to-face consult will provide the practitioner with the opportunity to conduct follow-up assessments and investigations, while adapting the treatment plan or appropriate referral. In the case of Achilles tendinopathy, this would include reassessment of hip strength and control and foot mechanics that are less easily completed with telehealth options.
The selection of consult options may not be static along the course of a client’s healthcare journey and the flexibility to adapt the method based on their presentation and preferences is a significant opportunity after an initial rapid uptake of telehealth by necessity.
How do we best move toward a tech-integrated model that works for both practitioners and clients?
Integrating technology with a long-term view of an updated service delivery model can seem like a daunting idea. What seems to be most important for the ultimate success or failure of telehealth and associated technology is practitioner acceptance (Cottrell & Russell, 2020). Encouragingly, evidence also shows that with training and repeated attempts, acceptance can change and practitioners can successfully adapt to this way of interacting with clients and delivering care (Cottrell & Russell, 2020).
Factors such as increasing practitioner confidence with technology and addressing practitioner concerns about safety, privacy and quality of care can all help a practitioner move toward acceptance (Cottrell & Russell 2020).
With increasing access to consumer-grade technology, reduced cost and increased speed of data, combined with unprecedented ability to reimburse telehealth consults (Cottrell & Russell 2020), the time has never been better to explore a sustainable, tech-integrated model that can optimise and individualise client care.
If you’re starting on your technology journey, it’s important to find what works for your clinic and your clients and to break down some of the barriers through training and giving things a go. While you do this, we urge you to consider how you can use technology to improve client care beyond the convenience of a telehealth appointment alone.
This article was originally published in Issue 19 of Allied Magazine.
Written by Mark Opar and Sjaan Gomersall.
References:
Cottrell, M & Russell, T, 2020, Telehealth for musculoskeletal physiotherapy, Musculoskeletal Science and Practice, 48, 102193. Essery, R, Geraghty, A, Kirby, Yardley, 2017, Predictors of adherence to home based physical therapies: a systematic review. 39, pp 519-534. O’Keefe, M, Hayes, A, McCreesh, K, Purtill, H, O’Sullivan, K, 2017, Are group-based and individual physiotherapy exercise programmes equally effective for musculoskeletal conditions? A systematic review and meta-analysis. BMJ Sports Medicine. 51; pp 126-132.
About Mark

Mark Opar is Head of Strategy for VALD Health. Mark has worked in private practice for eleven years using different technology solutions to improve client engagement and adherence and is on a mission to remove technical barriers around exercise prescription and improve client compliance.
About Sjaan

Sjaan Gomersall (PhD) is a Clinical Consultant at VALD Health and Senior Lecturer in Physiotherapy at The University of Queensland. Sjaan’s research expertise is in physical activity and health outcomes, with a particular focus on increasing adherence through understanding and implementing behaviour change techniques and translating these into clinical practice.
