Bringing Elite Sport Physiotherapy Care to the NHS
Available in:
EN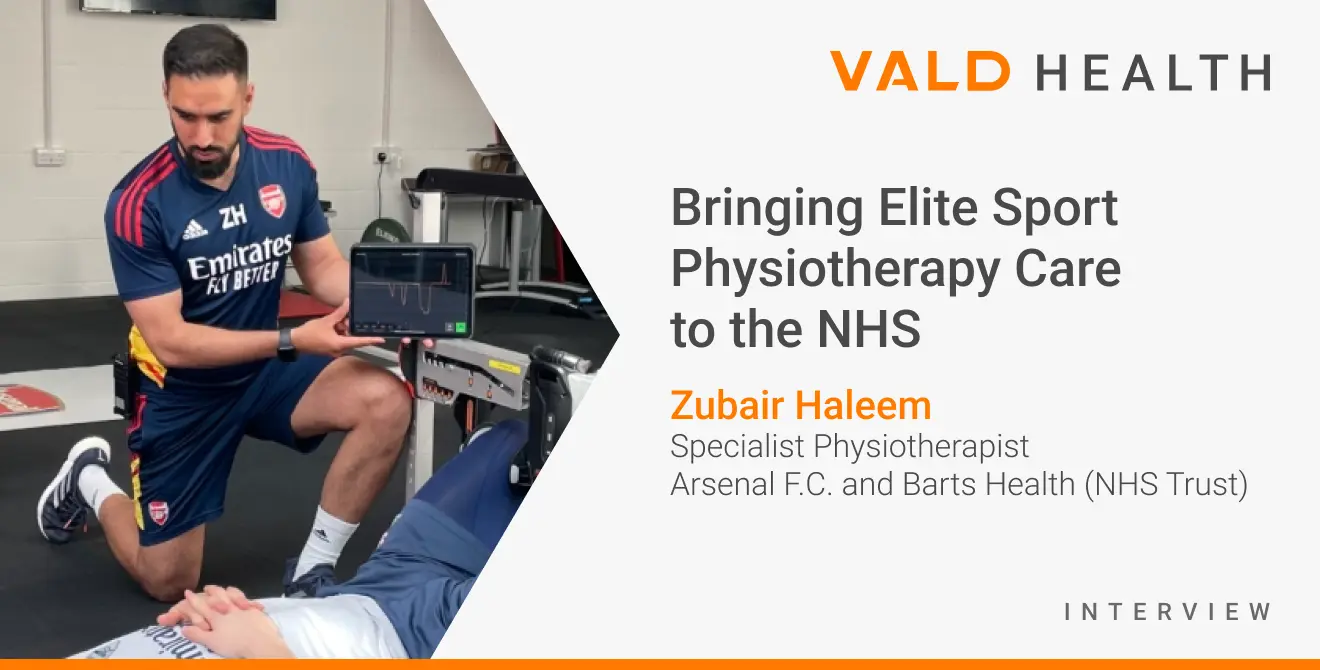
Zubair Haleem is a Specialist Physiotherapist with over a decade of experience in professional sport, research and outpatient musculoskeletal physiotherapy. He is currently a Senior Academy Physiotherapist at Arsenal F.C., a Senior Research Physiotherapist at Queen Mary University (London) and the Tendon clinic lead at Barts Health (NHS Trust).
We recently caught up with him to learn about how he’s bringing his experience with managing and rehabilitating elite athletes at Arsenal F.C. using VALD’s objective measurement technology to the NHS.
In this discussion, Zubair covers the benefits of objective measurements, why he uses VALD technologies, how he applies his learnings from elite sport rehabilitation to the general population, types of conditions it is suitable for and how it’s impacted him as a physiotherapist in his clinical decision making.
Zubair also provides some practical insights on how they were able to not only implement new technologies into clinical workflow, but also how to navigate the integration into a public health system.

Want to know how VALD can help you integrate objective measurement into your organisation? Please reach out below.
Key takeaways from Zubair:
- We often fail to measure: In clinic, we often prescribe ‘strengthening’ exercises but can fail to objectively measure whether our plans have resulted in any meaningful changes
- Testing in clinics is now possible and invaluable: The ability to quickly assess various measures of strength and force in a clinical setting has become invaluable in monitoring and progressing rehabilitation plans.
- Tracking progress: I now regularly use VALD system in my NHS clinics to inform, educate and track patients’ progress.
- Data informs decisions: Rehabilitation can be progressed or regressed based on objective measurement findings in conjunction with other clinical markers.
- Can be easily explained by patients and clinicians: The data visualisation provided by VALD systems can be easily explained by patients and clinicians.
- Something for all patients: I believe some level of testing and monitoring is indicated for the majority of patients to guide rehabilitation, regardless of diagnosis or joint involvement.
- Normative data in absence of diagnosis: In the absence of a definitive diagnosis, it can be important to identify areas to work on (or not to work on) if objective measures suggest they have suitable strength compared to normative data.
- Improved reliability, efficiency and accuracy: Inter-rater and intra-rater reliability of our manual muscle and ROM testing can be poor. Therefore, standardising testing with accurate measures – saved straight to a patient profile – can improve reliability and the service provided.
- Better patient insights: I feel the use of the VALD system provides me with a better understanding of the patient’s capabilities which then allows us to make informed collaborative decisions together.
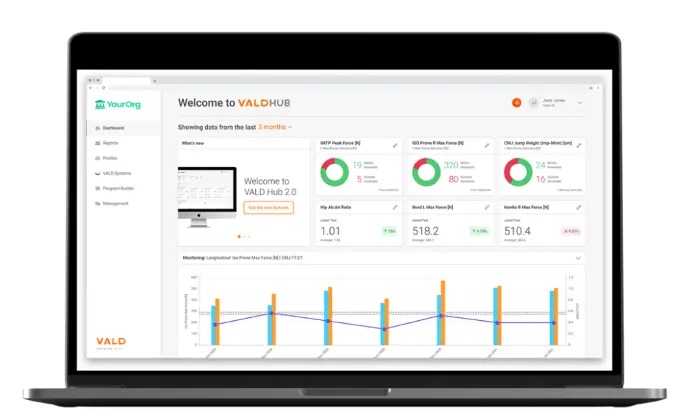
- Efficient processes: In a busy NHS clinic it’s essential to streamline processes for efficient use of time. The data storage and visualisation within VALD hub does most of the hard work for our team and allows us to maximise clinical time with the patient.
- Measure what you prescribe: If part of our role as physiotherapists is to build strength/ force generating capacity across muscles, tendons and joints then we should be able to accurately measure it.
- Future opportunities: Planning to roll the VALD systems out in our group-based exercise classes (OA Knee/ Hip, Upper limb class and back pain classes) as a means of visual feedback, training modality, track changes over time and to investigate associations with outcomes.
Why is using objective measurement technology important?
As physiotherapists, one of the goals during rehabilitation is to return the patient to their optimal strength following injury, however it can be difficult to assess whether you are objectively meeting your targets. In clinic, we often prescribe ‘strengthening’ exercises but can fail to objectively measure whether our plans have resulted in any meaningful changes. Isokinetic dynamometry testing can be a useful solution, but is expensive, challenging to set up and time consuming to complete. Over the years, smaller handheld dynamometers have been developed to bridge the gap however the ability to track changes over time with automated analysis remained limited.
In clinic, we often prescribe ‘strengthening’ exercises but can fail to objectively measure whether our plans have resulted in any meaningful changes.
When did you come across VALD technology?
I first started using VALD performance systems in my role with Arsenal F.C. with the ForceFrame, NordBord and ForceDecks. Since then, the ability to quickly assess various measures of strength and force in a clinical setting has become invaluable to me in monitoring and progressing rehabilitation plans. I now regularly use this equipment as well as the DynaMo Plus in my NHS clinics to inform, educate and track patients’ progress.
Is there a difference in how you use the systems between your elite sport setting and your community rehab setting?
We utilise these systems daily within an elite sports setting, alongside measures of wellness. We measure isometric peak force, jump height and rate of force development (RFD) within the fit squad to monitor fatigue, responses to previous sessions and readiness to train.
In a rehab setting, based on the stage of rehabilitation there may be a focus on a particular output such as eccentric strength or reactive strength index (RSI) that can be easily assessed. Rehabilitation can be progressed or regressed based on these findings in conjunction with other clinical markers.

What is the benefit of using VALD technology with general population?
I feel the use of VALD systems has enhanced my clinical practice within the NHS. Patients still need to master the basics, however providing them with a baseline, identifying deficits, implementing specific exercise plans through TeleHab and then re-testing objective measures alongside digital PROMs has assisted in streamlining processes and service delivery.
Patients are now increasingly using technology to enhance their own health and wellbeing. The data visualisation provided by VALD systems can be easily understood by patients and clinicians. The data collected can also help me identify patterns amongst groups in my patient demographic which helps inform service developments.
Patients are now increasingly using technology to enhance their own health and wellbeing. The data visualisation provided by VALD systems can be easily understood by patients and clinicians.

What type of patients or clinical presentations do you use these systems with?
I run a complex rehab and tendon clinic within the NHS, the aim of which is to:
- confirm diagnosis where possible;
- ensure rehabilitation has been optimised; and
- consider alternative treatment strategies.
I believe some level of testing and monitoring is indicated for the majority of patients to guide rehabilitation, regardless of diagnosis or joint involvement, and I have used VALD systems for patients with both upper and lower limb complaints.
In the absence of a definitive diagnosis, it can be important to identify areas to work on (or not to work on) if objective measures suggest they have suitable strength compared to normative data. For example, I would typically profile a patient with a lower limb complaint using the following tests:
- Hip abduction/adduction (ForceFrame);
- Knee flexion/extension (DynaMo);
- Ankle plantar flexion (ForceFrame); and
- Jump testing on ForceDecks, where appropriate.
In the absence of a definitive diagnosis, it can be important to identify areas to work on (or not to work on) if objective measures suggest they have suitable strength compared to normative data.

In terms of future opportunities, I’m currently planning to roll the VALD systems out in our group based exercise classes (OA Knee/ Hip, Upper limb class and back pain classes) as a means of visual feedback, training modality and to track changes over time.
What are some of the general key metrics you look at:
The metrics I focus on are largely dependent on the patient in front of me. It can be easy to get carried away with the data, and therefore clinical reasoning is always imperative. Here are some examples:
- Acute stage rehabilitation: I may choose to complete sub-maximal isometric training in a pain-free, safe range to maintain function and reduce atrophy.
- End-stage shoulder rehabilitation: I may look at peak isometric force of external rotation in a overhead position or look at rate of force development in an I-Y-T ASH test protocol.
- A runner with achilles tendinopathy: I may want to look at double or single-legged plyometric movements on ForceDecks, with attention to jump height, peak landing forces, side-to-side asymmetries, reactive strength or ground contact times. Deficiencies in any of these metrics can prompt me to make adaptations to plans.

How has VALD technology impacted your clinical decision making compared to traditional assessments?
I believe the core key principles of physiotherapy assessments shouldn’t change. A thorough subjective examination, listening to the patient’s thoughts, beliefs and expectations alongside a comprehensive objective examination should result in a sound understanding of the person.
However, we know that the inter-rater and intra-rater reliability of traditional manual muscle and ROM testing can be poor. Therefore, standardising testing with accurate measures – saved straight to a patient profile – can improve reliability and the service provided. I feel the use of the equipment provides me with a better understanding of patients’ capabilities, which then allows us to make informed, collaborative decisions together.
However, we know that the inter-rater and intra-rater reliability of traditional manual muscle and ROM testing can be poor. Therefore, standardising testing with accurate measures – saved straight to a patient profile – can improve reliability and the service provided.

How do you incorporate these systems into your clinical workflow?
The plans we have start with a link to VALD systems, which we created within our existing NHS CRS system. This should allow for patient’s testing, home exercise programmes and PROMs to be easily accessible alongside the patient’s medical notes and records in one central location.
In a busy NHS clinic, it’s essential to streamline processes for efficient use of time. The data storage and visualisation within VALD hub does most of the hard work for our team and allows us to maximise clinical time with the patient.
The data storage and visualisation within VALD hub does most of the hard work for our team and allows us to maximise clinical time with the patient.
What were some of the barriers to introducing these systems at an NHS trust and how did you overcome these?
Inevitably, there are always barriers and challenges to introducing new systems within the NHS. Data protection within the NHS is paramount, so it is essential that the relevant checks and agreements are in place prior to roll out. This can be a lengthy process but regular communication and meetings with respective clinical governance, workflow and ICT teams at the trusts can help facilitate implementation.
However, through practical teaching sessions and education, therapists became more comfortable, inquisitive and realised the multiple benefits for patients within the NHS.
At the ground level, there can also be resistance to change due to fear of using new technology, knowledge limitations and scepticism regarding the benefits over traditional care. For example, some members of the department initially felt the equipment was only suitable for sportspeople. However, through practical teaching sessions and education, therapists became more comfortable, inquisitive and realised the multiple benefits for patients within the NHS.
The equipment doesn’t make you a better clinician, but does encourage you to be more accountable with exercise prescription, and to target specific physiological adaptations where necessary. It also helps shift responsibility onto the patient, to help them meet their goals. If part of our role as physiotherapists is to build strength (force generating capacity) across muscles, tendons and joints, then we should be able to accurately measure it.
What other applications are you planning for VALD systems?
We are currently piloting the use of strength testing, TeleHab exercises and PROMs in our OA Classes to see if we see changes in pain, strength, adherence and function compared to our conventional class system.

Want to know how VALD can help you integrate objective measurement into your organisation? Please reach out below.
