How technology can leverage behaviour change science to increase adherence to home exercise programs
Available in:
EN
Article by Dr. Sjaan Gomersall,
Senior Lecturer in Physiotherapy, University of Queensland;
Clinical Consultant at VALD.
It is now well established that exercise is a mainstay of evidence-based musculoskeletal rehabilitation, with the vast majority of therapeutic exercise prescribed as home exercise programs. The intention is that clients complete these programs at home independently between real-time consultations (either face-to-face or via telehealth), typically without supervision from health professionals or the peer-support that may come from a group setting. Despite the fact that we know exercise largely ‘works’, the rates of exercise program completion are incredibly low (as low as 30%; Essery et al. 2017). Trying to find ways to improve client adherence with exercise prescription, and subsequently improve their outcomes, has been receiving an increasing amount of both practitioner and researcher attention.
At the same time, the availability of technology that can be accessed in day-to-day clinical operations has been increasing, and the sophistication of that technology has been improving rapidly. There are many ways that technology can be harnessed to address the adherence problem, but the important questions are how, for whom and how much – and what is the right balance for the right person. There is simply no ‘one size fits all’ approach to the low rates of adherence, as with many clinical problems. To give some structure to these decisions and how they are applied in practice, many researchers have started looking toward behavioural science for what is, fundamentally, a behaviour change challenge.
Behaviour change approaches acknowledge the complex interactions between the individual and their environment, both physical (e.g. places and locations) and social (e.g. friends and family). Taken together, these factors ultimately influence whether or not they perform an intended behaviour (e.g. completing home exercises), and how this then influences the desired health outcome (e.g. muscular strength or endurance). There have been a number of theories or frameworks in behavioural science, but none that have had the impact of the Behaviour Change Wheel and the associated Behaviour Change Technique Taxonomy. At its centre, the Behaviour Change Wheel proposes that an individual must have the capability, opportunity and motivation in order to change their behaviour (Michie et al 2011). The complimentary Behaviour Change Technique Taxonomy is an evidence-based compilation of 93 behaviour change techniques, or active ingredients for change. This provides people designing or reviewing interventions with a suite of strategies to choose from and a common language (Michie et al 2013).
To what extent do exercise professionals already implement behaviour change into day-to-day practice?
While the language and frameworks of behaviour change may be relatively new to this problem, exercise professionals use aspects of these approaches in clinical practice every day. For example, a group of researchers (Kunstler et al. 2019) surveyed almost 600 Australian physiotherapists and, using the 93 behaviour change techniques as a framework, asked them to rate which technique they used to promote non-treatment physical activity and rehabilitation exercises for clients with musculoskeletal conditions and how often they used them. For rehabilitation exercises, graded tasks was the most frequently reported technique, followed by body changes, reward approximation and social reward.
This effectively means that when it comes to behaviour change in practice, practitioners are more likely to use a progressive rehabilitation program, that is focused on the physiological changes that will result (e.g. changing muscular strength), with a verbal or non-verbal reward (e.g. positive reinforcement) when there has been effort and progress toward exercise completion. Overall, physiotherapists reported using 28 of the 93 behaviour change techniques, either infrequently, about half of the time or frequently.
How can technology be used to implement behaviour change strategies and improve client adherence?
Although practitioners indicate that they use a reasonable range of behaviour change strategies, given the reportedly low adherence rates and the unequivocal evidence for the efficacy of exercise for musculoskeletal conditions, it is worth exploring whether novel approaches may be integrated into day-to-day practice. The increase in accessibility and range of digital health technologies, for both clients and practitioners, offers considerable opportunity for the implementation of behaviour change strategies which previously were either too cumbersome and/or resource intensive to be practical. For example, smartphones and wearable devices offer a range of opportunities for supporting clients with behaviour change strategies between real-time consults. These may include self-monitoring of the behaviour (i.e., tracking or logging exercise sessions), monitoring of behaviour by others with or without feedback, (i.e., sharing sessions with practitioners), prompts/cues (i.e. real-time or general reminders about when clients are to complete their exercises), or by enhancing patient education focused techniques like information about health consequences, through the ability to push educative materials efficiently and in cost-effective ways.
TeleHab Exercise Prescription App incorporates a range of behaviour change techniques for practitioners to support their clients to increase adherence to home exercise programs. Most recently, this has included the introduction of notifications, where clients receive either general, or real-time prompts or cues to remind them to perform their home exercise, based on their prescribed schedule.
There is good evidence for this approach to increase adherence to exercise. A systematic review and meta-analysis synthesised evidence from 20 trials aiming to increase physical activity demonstrated that prompts and cues were an effective behaviour change strategy in healthy, but inactive adults (Howlett et al 2019). There is also evidence for these approaches in the musculoskeletal rehabilitation context, with an increase in exercise adherence for knee (Bennell et al 2020) and shoulder rehabilitation (Chen et al 2017) and from our own work in exercise oncology (Gomersall et al 2019).
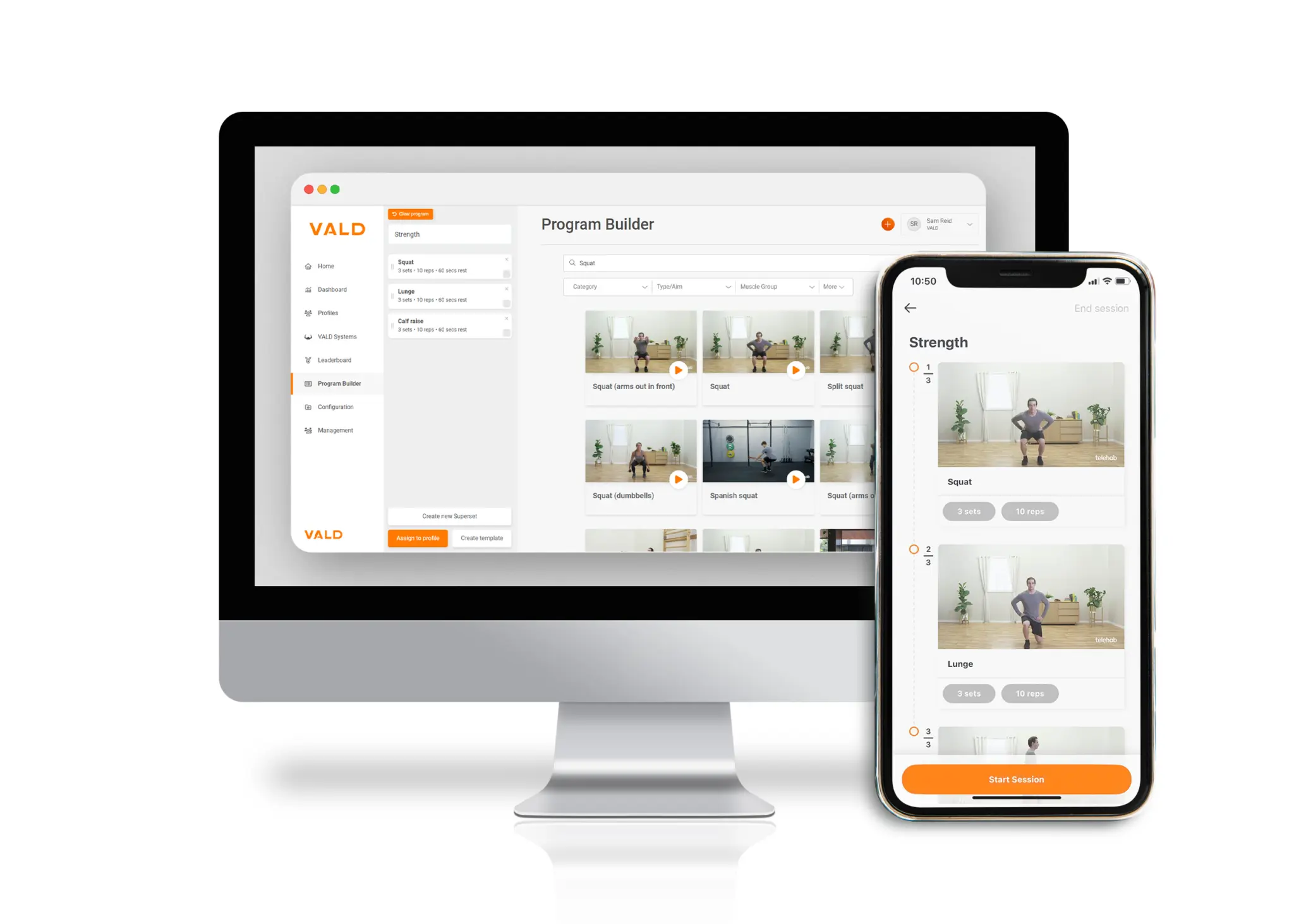
The scheduler and notifications features in TeleHab provide some of the first practical, automated, but also individually tailored prompts and reminders that practitioners can use in practice. The combination of scheduling, plus the associated notifications enable practitioners to support their clients to complete their home exercise programs between real-time consults. Maybe most importantly though, the inclusion of schedules and notifications at the point of home exercise program prescription provides the practitioner with an opportunity to start a dialogue about exercise adherence with their client and to collaboratively come up with a plan that will set them up for success.
If you would like to sign up or log into TeleHab (for free), please see below.
References
Bennell, K, Nelligan, R, Schwartz, S, Kasza, J, Kimp, A, Crofts, S, Hinman, R. 2020. Behavior Change Text Messages for Home Exercise Adherence in Knee Osteoarthritis: Randomized Trial. Journal of Medical and Internet Research. Vol. 22, issue 9.
Chen, H, Chuang, T, Lin, P, Lin, Y, , Chuang, Y. 2017. Effect of messages delivered by mobile phone on increasing compliance with shoulder exercises among patient with frozen shoulder. Journal of Nursing Scholarship. Vol 49, issue 4, pp. 429-437.
Essery, R, Geraghty, A, Kirby, Yardley, 2017. Predictors of adherence to home based physical therapies: a systematic review. Disability and Rehabilitation. Vol. 39, issue 6, pp 519-534.
Gomersall, S, Skinner, T, Winkler, E, Healy, G, Eakin, E, Fjeldsoe, B. 2019. Feasibility, acceptability and efficacy of a text message-enhanced clinical exercise rehabilitation intervention for increasing ‘whole-of-day’ activity in people living with and beyond cancer. BMC Public Health. Vol 19, supp 2.
Howlett, N, Trivedi, D, Troop, N, Chater, A, 2019. Are physical activity interventions for healthy inactive adults effective in promoting behavior change and maintenance, and which behavior change techniques are effective? A systematic review and meta-analysis. Translational Behavioural Medicine. Vol. 9, issue 1, pp 147-157.
Kunstler, B, Cook, J, Kemp, J, O’Halloran, P, Finch, C. 2019. The behaviour change techniques used by Australian physiotherapists to promote non-treatment physical activity to patients with musculoskeletal conditions. Journal of Science and Medicine in Sport. Vol. 22, pp 2-10.
Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011 Apr 23;6:42
Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013 Aug;46(1):81-95.
See below for other news and articles on TeleHab:
📚 What will telehealth’s future look like post-COVID-19?
📚 Finding the balance between prescribing home exercise programs for adaptation and adherence
