Digital Health 101: Connecting, streamlining and improving care
Available in:
EN
What Is Digital Health?
We define “digital health” as using technology-enabled solutions to support, enhance and improve patient care. This description is a modified version of the definition offered by the World Health Organization.
At its heart, digital health is about connecting health professionals and patients using digital measurement tools and data to improve healthcare delivery and clinical workflow efficiencies.
At its heart, digital health is about connecting health professionals and patients…
Digital health is changing the way clinicians and patients interact with clinical care and rehabilitation.
Digital health is not intended to replace in-person care with technology. While there are aspects of everyday clinical life that are benefiting or will benefit from automation, it is about using technology as an enabler to support, augment and enhance aspects of care. Places where digital health is making a positive impact — specifically for physical therapists, physiotherapists and any musculoskeletal specialists — include clinical decision-making, clinical workflows, patient engagement and treatment efficacy.
Digital health is not intended to replace in-person care with technology …it is about using technology as an enabler to support, augment and enhance aspects of care.
Digital health technology comes in many forms, including:
- Clinic Management Software: Practice/patient management system (PMS) and electronic medical/health record (EMR/EHR)
- Mobile Health Apps: Home exercise program (HEP) to prescribe exercise programs and offer patient education on the program assigned
- Objective Measurement Technology: Sensor-based clinical assessment technologies
- Telehealth: Virtual consultations
- Web-based Information Provision: Internet search engines and artificial intelligence (AI)-powered large-language models
- Remote Monitoring Sensors: Wearables and other remote monitoring devices
- Questionnaires: e.g., digital patient reported outcome measures (PROMs)
- AI-Powered Tools: e.g., clinical note transcription
- Virtual and Augmented Reality: Used to enhance therapeutic intervention delivery
- Cloud-based Clinical Data Management: Dashboards, portals and data analytics platforms
In the coming years, as digital technology becomes inextricably linked to care, we anticipate that the terms “health” and “healthcare” will inherently encompass these aspects – there will no longer be any need to refer to it as digital health.
How Does It Work?
Digital health can be woven into most aspects of everyday clinical treatment of patients and athletes and can be integrated into many aspects of how a clinic operates.
| Steps | Digital Health Tool | |
|---|---|---|
| 1 | Patient makes an appointment |
|
| 2 | Pre-consult forms |
|
| 3 | Initial patient evaluation |
|
| 4 | Remote monitoring |
|
| 5 | Follow-up appointments |
|
A Worked Example of Digital Integration
Patient Booking and Record Creation: These are managed via a PMS or EMR. Patients book their consultations with the practice via an online portal that manages the workflow and patient records.
Pre-Consultation Questionnaires and PROMs: Via an app, the clinician sends a questionnaire to the patient to assess their health status and introduce them to their digital access point for all their data, such as the MoveHealth app. All of this feeds back into a central data platform like VALD Hub.
In-Person Evaluation: During the consultation and in conjunction with a typical clinical assessment, objective measurement technology (e.g., DynaMo, ForceDecks, ForceFrame, NordBord, HumanTrak and SmartSpeed) is used to conduct relevant tests to improve the clinical assessment and gain better data-informed insights, particularly through the use of normative data.

In-session testing delivers real-time results and tracks patient progress to drive better engagement and outcomes.
Post Consultation: The patient is then allocated a customized, visual HEP along with educational content on their condition, as well as a PROM to complete at a specified time, all accessed through a patient app. Compliance and feedback regarding the program are remotely monitored by the clinician. In some instances, feedback between patient and clinician is possible, keeping everyone up to date in real time. Patient progress is recorded using an AI note taker, saving the clinician time and delivering accurate consultation notes.
Ongoing Care: Once a follow-up appointment is made, the clinician can retest the patient and, if required, re-do the PROM questionnaire. After reassessing the patient, the existing HEP can be quickly updated to reflect the changing needs of the patient.
By embracing digital tools, clinicians get access to better quality data and objective measurements to inform clinical decisions…
While this is a broad example of the practical application of digital health in a clinical environment, it demonstrates the value technology can offer both the clinician and the patient. By embracing digital tools, clinicians get access to better quality data and objective measurements to inform clinical decisions, saving time and ensuring that the patient is better connected throughout their treatment, even when they leave the practice.
How Can Digital Health Impact Your Workflows?
When applied correctly, digital health reduces the administrative burden on clinicians and the admin team, making the practice more efficient and allowing clinicians to provide a better quality of service to their patients.
- Reducing Administrative Burden and Workload: Digital tools can help automate, streamline or even eliminate documentation, PROM collection, exercise prescription, invoicing and analytical reporting.
- Simplified Stakeholder Communication: By creating a cohesive digital environment, multiple stakeholders can access the same information, encouraging consistent communication and reducing duplication that can become tiresome for the patient.
- Improving Patient Flows: Online bookings, digital appointment scheduling, recalls, forms, communication and reminders are all features that can help save time and reduce appointment no-shows.
- More Seamless Data Integration: Connected systems ensure that assessment data, rehab plans, outcomes, imaging and progress tracking are easily accessible.
- More Precise Treatment Planning: Real-time and near-real-time patient monitoring and AI-powered clinical insights can enhance clinical decision-making.
- Early Intervention, Risk Stratification and Prevention: Digital health tools can be used to flag concerns or trends in patient-reported data or highlight when a patient’s results fall outside expected normative values, prompting individualized, timely clinical actions.
Connected systems ensure that assessment data, rehab plans, outcomes, imaging and progress tracking are easily accessible.
Implementing digital health tools will initially require a time investment from the business, including learning and onboarding with the new systems. However, this initial investment in time is typically well worth the effort for long-term time savings. Systems can be implemented gradually, allowing the digital health ecosystem to grow as clinicians become more comfortable with the systems and technology.
Selecting the Right Digital Health Tools for You
Not sure where to start? Begin by assessing your clinical needs. Having a specific staff member to champion these changes can be a huge help, as well as starting with a subset of your patients before rolling it out to all patients. Ensure everyone knows why and how you are using these tools.
Here are some digital health tools to consider starting with:
Digital Home Exercise Programs
HEPs are a cornerstone of digital health tools, with handwritten instructions and Excel spreadsheets now a thing of the past.
The delivery of HEPs via digital platforms is becoming the expectation of patients as on-demand access becomes the standard across multiple industries. While there is a learning curve for a new platform to create HEPs, the time saved in the long run and the benefit to the patient is immeasurable.
The delivery of HEPs via digital platforms is becoming the expectation of patients…
For example, MoveHealth is VALD’s digital health platform that allows clinicians to remotely monitor their patients’ exercise and outcome measures and is available to all clinicians for free.
Digital HEPs are easy to assign, quick to complete and convenient to monitor. Clinicians can build exercise programs with MoveHealth’s intuitive and flexible program builder, then prescribe them directly to their patients’ iOS or Android devices at the press of a button.
Clinicians are able to assign programs through VALD Hub's home exercise program builder. Patients are stepped through their exercises by a simple, easy-to-understand interface, including push notification reminders, with their results immediately available to them in-app and automatically updated in their VALD Hub profile for clinicians to monitor.
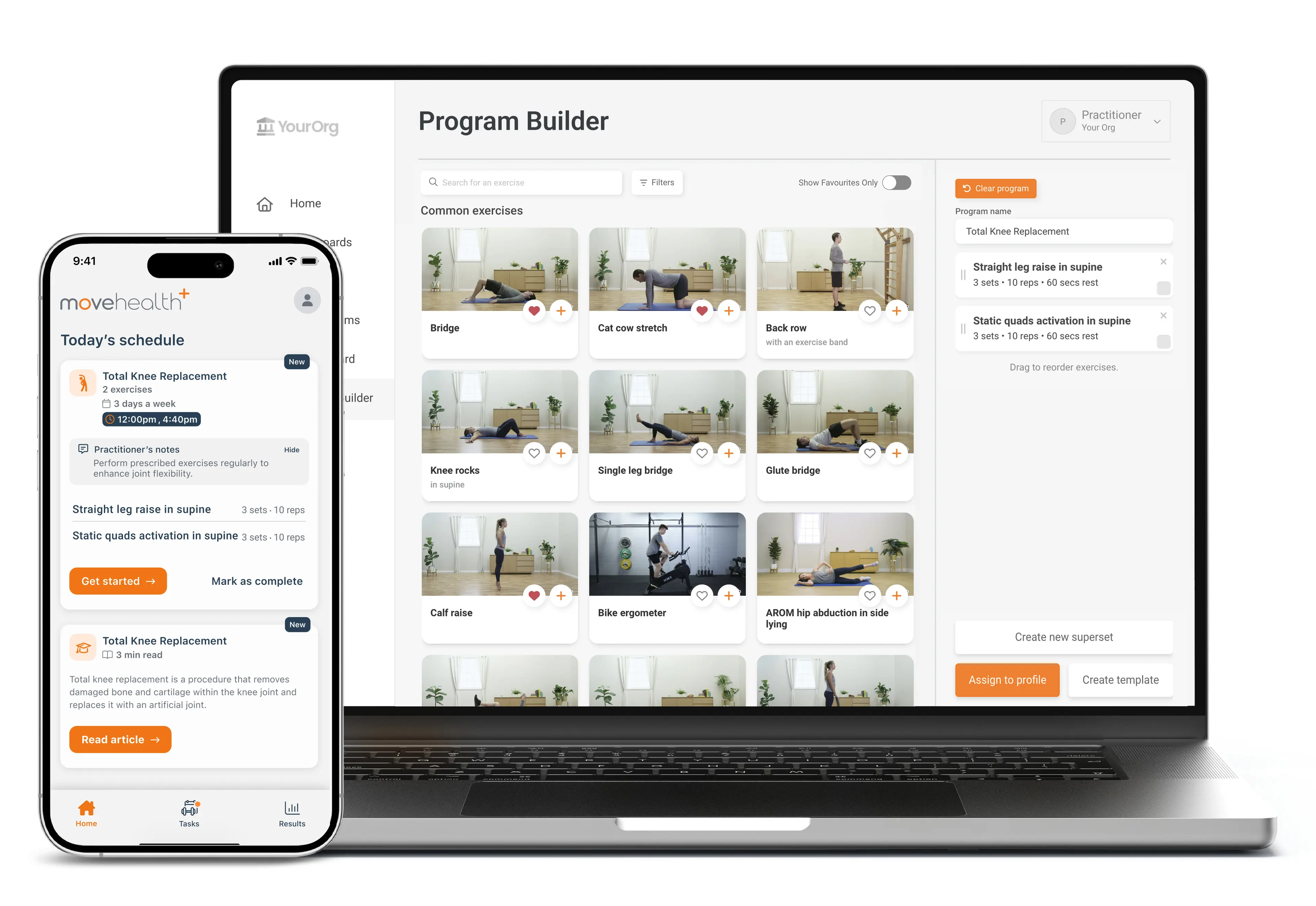
Combining VALD Hub and MoveHealth gives the clinician and patient an effective and accurate video-led HEP solution.
Normative Data, Powered by VALD
Showing a patient how they have performed against relevant normative data is one of the first steps in giving them the tools to take control of their health. Norms allow them to understand how they compare to their peers and allow them to better understand and comply with their treatment plan.
Showing a patient how they have performed against relevant normative data is one of the first steps in giving them the tools to take control of their health.
VALD Norms (normative data) integrated into VALD Hub.
MoveHealth leverages VALD’s integrated Norms, directly overlaying population-specific normative ranges onto patients’ results, giving you and your patient instant context about their movement health.
Patient Reported Outcome Measures
Measurement tools such as PROMs can be used to determine a patient’s self-assessed health status at a particular point in time and are increasingly recognized as providing valuable and essential information for achieving health goals. Recording the patient’s perspective allows the clinician to assess how the quality of their care is perceived and is considered essential to a patient-centered approach.
Platforms that deliver freeform questionnaires can yield unreliable and inconsistent results when not administered consistently.
Alongside VALD’s HEP builder, VALD Hub includes a range of well-researched, validated PROMs that can be assigned with a click, ensuring patients’ PROMs data is accurate and reliable, with automated follow-ups to capture change over time. Clinicians can then review the individual response to inform and update the treatment plan.
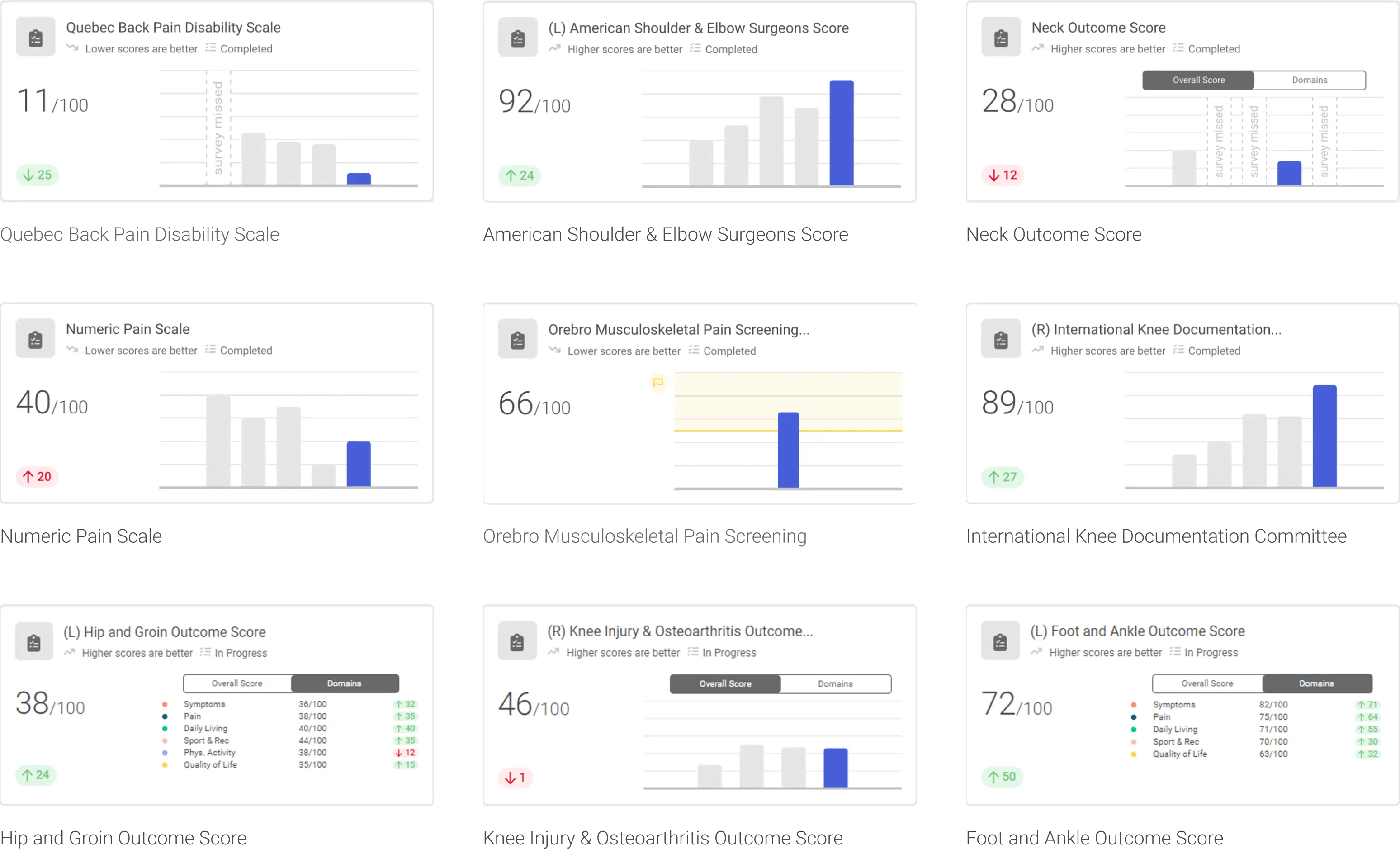
Validated, research-backed PROMs in VALD Hub provide accurate and reliable patient-reported outcomes to support personalized, patient-centered care.
Patient Education
When patients understand the “why,” they are more likely to do the “what.”
In a traditional consultation, patient education is often rushed due to time constraints. Kessels (2003) shows that most of the medical information discussed in a session is immediately forgotten or recalled incorrectly.
However, with VALD Hub, clinicians can assign more than 140 relevant educational topics that can easily be shared with their patients via the MoveHealth app. When patients get the right message about their condition, they can understand what they might experience during their rehabilitation or management journey.
When patients get the right message about their condition, they can understand what they might experience during their rehabilitation or management journey.
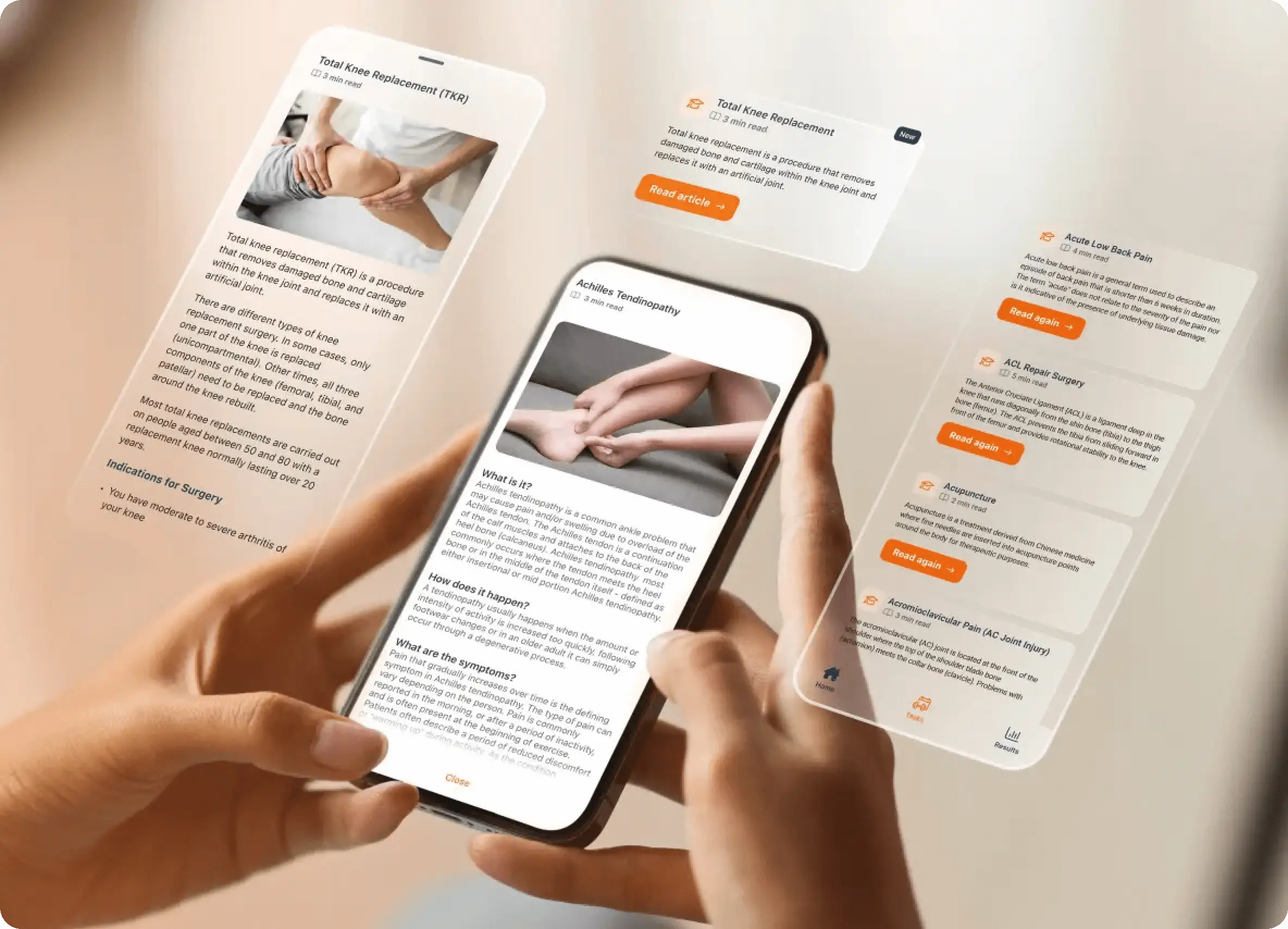
Learn about your recovery with accessible educational content, helping you stay engaged, informed and aligned with your rehabilitation goals.
Digital education delivered through the app is also highly effective, as it removes the need for patients to rely on memory from information-heavy consultations.
The MoveHealth app allows patients to read about their condition at a later stage and refer back to it as often as needed.
Objective Measurement Tools
Objective measurement tools help clinicians measure a patient's progress and allow for more accurate, data-informed treatment decisions. The results give the clinician accurate and actionable insights. They can also be used to track a patient's progress over time and are key to informing the evolution of their HEP.
Objective measurement tools help clinicians measure a patient's progress and make more accurate, data-informed treatment decisions.
VALD technology provides unparalleled insights to health and performance professionals, and having objective measurement results alongside our extensive normative data pool enables better use of digital health tools and improves patient care.
Why Embrace Digital Health?
There are many benefits to using and implementing digital health tools. Irigoyen (2024) overwhelmingly suggests that technology and AI will play a huge role in the healthcare space. Some of the benefits of embracing digital health include:
- Facilitating Multi-Disciplinary Collaboration: Being able to share data across teams and team members puts the patient at the center. It will enhance coordinated care, reduce redundancies, improve patient satisfaction and ultimately improve health outcomes.
- Encouraging Patient Accountability: Digital tools aim to foster self-management and engagement from patients to take on a more active role in their own care.
- Meeting Evolving Patient Needs and Expectations: As healthcare continues to evolve in the digital age, patients increasingly expect digital options as part of their healthcare experience.
- Responding to Health System Challenges: While this will always be regionally specific and jurisdictional, digital solutions can support some of the common challenges experienced in the health system: clinician shortages, patient access barriers and system inefficiencies.
- Preparing for the Workforce of the Future: Upskilling in digital health will position clinicians as leaders in technology and innovation. This is increasingly important as the workforce matures and healthcare is increasingly influenced by technology.
Digital health provides the platform for a better-educated and empowered patient with a higher likelihood of seeing positive rehabilitation outcomes.
How Can Digital Health Transform Your Business?
Digital health offers the opportunity to provide more effective, data-informed and accurate care while improving in-clinic efficiency. It allows for a more engaged and empowered patient, which inevitably delivers a higher level of compliance with rehabilitation programs.
Digital health…allows for a more engaged and empowered patient, which inevitably delivers a higher level of compliance with rehabilitation programs.
The powerful combination of digital health and effective measurement tools helps patients stay connected to their care and take a more active role in their recovery. When combined with VALD’s Norms, it will allow clinicians to instantly compare patients to age- and sex-matched norms and visualize their progress through the data.
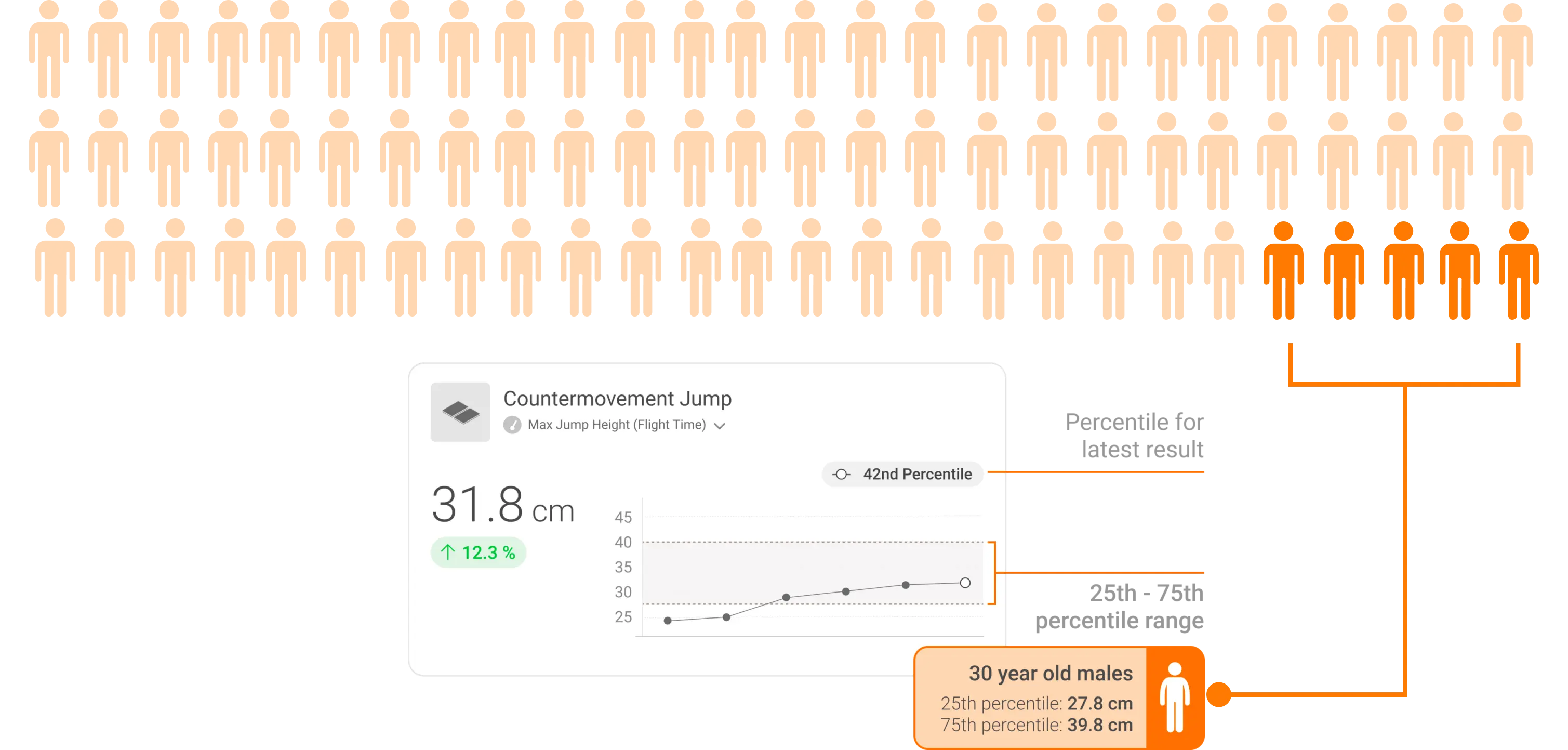
Visualizing patient performance against age- and gender-matched Norms and percentiles to support data-informed care and patient engagement.
The adoption of effective digital health tools can lead to better patient engagement, more effective consultations and – most importantly – better patient outcomes. Using clear, visualized data relevant to the patient is a key driver of patient retention.
Data-informed observations mean it is not the clinician telling them they need ongoing treatment; the data, especially when combined with VALD’s normative data, shows them.
The healthcare industry is going digital, but we are here to help you navigate these changes.
If you would like to find out more about how VALD's digital health products can help your business, your clinicians and your patients, get in touch.
References
- Kessels, R. P. C. (2003). Patients’ memory for medical information. Journal of the Royal Society of Medicine, 96(5), 219–222. https://doi.org/10.1258/jrsm.96.5.219
- Irigoyen, F. (2024). Physical therapy rehabilitation centers in the US (Report No. OD6047). IBISWorld. https://www.ibisworld.com
