The Sit-to-Stand Test: A key assessment tool in modern rehabilitation and fitness
Available in:
EN
For decades, the Sit-to-Stand (STS) test has been a cornerstone in clinical assessment. Simple yet profoundly impactful, the STS test demonstrates how foundational movements can reveal complex health insights, standing the test of time in the field of physical assessment.
This article unravels the intricacies of the STS test, highlighting its significance in both clinical and fitness settings, and how technology such as ForceDecks is enhancing its application.
What is the Sit-to-Stand Test?
The STS test is more than a simple strength and functional movement assessment. It is a fundamental yet deceptively complex action requiring muscle coordination, balance and endurance. This test has become a clinical standard with several variations:
- 30-Second Sit-to-Stand Test (30STS) – how many repetitions can be completed within 30 seconds?
- 5-Repetition Sit-to-Stand Test (5STS) – how quickly can 5 repetitions be completed?
- “Functional” Sit-to-Stand Test (FSTS) – assessment of the ability to perform the task and the quality of the movement (for example asymmetry, range of movement (ROM) and movement quality).
The 30STS and 5STS produce functional capacity scores that can be benchmarked against cohort normative data. Where the FSTS assesses the quality of movement and is used by practitioners to inform intervention programs.
The 30STS and 5STS produce functional capacity scores that can be benchmarked against cohort normative data. Where the FSTS assesses the quality of movement and is used by practitioners to inform intervention programs.
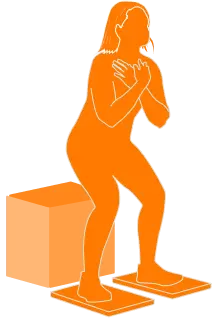
The FSTS can also be performed with technology, such as force plates, to measure a range of factors that cannot be determined by eye. As well as being more efficient – requiring as little as one repetition – performing the FSTS with force plates can provide more specific information than traditional tests, which can be used to inform targeted interventions. Metrics such as force production, asymmetry, rate of force development (RFD), time to sit and time to stand can all be used to develop intervention plans and monitor progress over time.
What is the value of the Sit-to-Stand Test?
Sitting and standing, fundamental yet often overlooked movements, are critical markers of functional mobility, particularly in older adults. These actions are integral to daily routines e.g., getting up from chairs, beds or toilets demanding specific lower body strength and balance. The test not only offers a concise but comprehensive overview of a patient's physical health and autonomy but also serves as a critical marker for:
- Early Detection and Preventative Measures: The STS test aids in identifying physical impairments, declining functions and muscle weakness early, enabling timely preventative strategies – decreasing risks of further physical decline.
- Assessment of Falls Risk: Vital in the care of older adults, the STS test accurately assesses falls risk, informing the development of targeted fall prevention programs for patients scoring poorly on the test.
- Personalization of Exercise Programs: Results from the STS test are instrumental in creating individualized rehabilitation programs, typically focusing on enhancing lower body strength, endurance, balance and overall functional mobility.
- Rehabilitation and Progress Monitoring: In clinical settings, the STS test benchmarks progress, helping practitioners quantifiably track recovery and the effectiveness of interventions.
- Patient Empowerment: The STS test motivates individuals by providing tangible, quantified progress that encourages participation and adherence to treatment plans.
- Enhancing Objective Measurement: Integrating technology such as ForceDecks can enhance the precision and value of the STS test. This technology can measure what traditional tests cannot – unlocking more detailed analysis like limb asymmetry, forces, power, speed and depth of squat enriching the data and insights from the test. The unique ForceDecks Vision even allows synchronized force data and video to be recorded and automatically annotated, providing a comprehensive recording of the patient’s performance.
Integrating technology such as ForceDecks can enhance the precision and value of the STS test ...unlocking more detailed analysis like limb asymmetry, forces, power, speed, and depth of squat enriching the data and insights from the test.
Who Would Benefit from Using the Sit-to-Stand Test
The STS test is versatile, catering to a wide range of patients, each with distinct needs and goals:
Adults: The STS test is a critical metric for assessing functional strength and mobility, particularly in sedentary patients. It enables early detection of deficits in lower limb muscular endurance and balance – crucial for injury prevention and occupational health. Regular STS test assessments can guide interventions to mitigate musculoskeletal decline, essential in maintaining workforce productivity and overall physical well-being.
Older Adults/Geriatric: STS testing is a significant tool for assessing and managing mobility, independence, falls risk and the need for specific interventions among older adults – helping to maintain their quality of life and reducing injury risks.
Orthopedic Patients: Beneficial for patients with conditions such as osteoarthritis (OA), knee- and hip replacements and more, the STS test provides quantitative progress measures, essential for customizing rehabilitation programs and ensuring optimal recovery outcomes.
Chronic Disease Patients: In chronic disease management, the STS test provides objective data on functional capacity impacted by conditions e.g., cardiovascular diseases (CVD), chronic obstructive pulmonary disease (COPD), stroke, etc. It aids in quantifying the effect of chronic illnesses on musculoskeletal health – guiding targeted rehabilitation strategies. Consistent use of STS testing allows for monitoring functional progress, essential for adjusting treatment plans and enhancing patient compliance and motivation in long-term disease management.
Neurological Patients: For patients with neurological conditions such as Parkinson's, Alzheimer’s, multiple sclerosis (MS) or traumatic brain injuries, the STS test can be invaluable. STS testing assesses functional mobility, balance and neuromuscular control of the lower limbs – which are often affected by these disorders. Regular STS test assessments help identify specific motor function limitations and track changes over time. This is critical for developing focused rehabilitation strategies aimed at enhancing motor skills, improving balance and increasing daily activity independence. Additionally, the STS test is useful in predicting falls risks – guiding proactive interventions in neurological rehabilitation.
Athletes: By adding external load or assessing function in early post-operative cases, athletes can leverage the STS test to evaluate and enhance their lower body strength and endurance, which are essential qualities to progress into higher levels of performance in many sports. These metrics can serve as early rehabilitation guardrails to ensure the athlete is improving and able to progress to more intense activities.
How to Perform the Sit-to-Stand Test
Despite the variations of the STS test, each has a similar protocol. The key difference is that in the timed tests such as 30STS and 5STS, the repetitions are completed as quickly as possible (respecting safety limitations), whereas the non-timed tests keep the focus on task execution and form.
Equipment Required:
- Sturdy chair (ideally 17 inches/43 cm height) with a backrest and no armrests.
- Stopwatch or timer (if performing a test for time).
Pre-test Procedure:
- Demonstrate the task and ensure the person is familiar with the task.
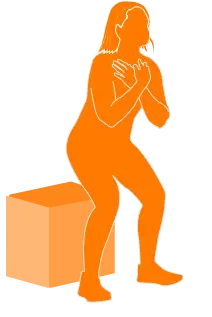
Starting Position:
- Position a chair against a wall or sturdy object to prevent movement during the test.
- Sit upright in the middle of a chair.
- Cross your arms over your chest.
- Place your feet flat on the ground (hip-width apart).
Test Procedure:
On instruction, lean forward – aligning your nose over your toes – then powerfully extend your hips, knees and ankles to assume a standing position and repeat to return to a seated position.
- For 30STS: Start the stopwatch or timer as soon as the patient initiates getting up, counting and keeping a record of the number of repetitions being performed until 30 seconds have passed.
- For 5STS: Start the stopwatch or timer as soon as the patient initiates getting up, then stop the stopwatch or timer after the completion of 5 repetitions.
- For FSTS: Complete a pre-determined number of repetitions, assessing the individual’s normal execution of the STS task.
Scoring and Interpreting the Results
In evaluating the results of the 30STS and 5STS, practitioners measure the repetitions and times, aiming to understand the implications of these numbers on a patient's lower body functionality.
| Test | Standard Metric | What it Means | Expected Progression |
| STS | Time to Complete 5 Repetitions | Amount of time the client takes to stand up and sit back down five times. | Time should decrease as strength and power improve. |
 | Number of Repetitions Completed in 30s | How many times the client can stand up and sit back down within 30 seconds. | Repetitions should increase as strength and power improve. |
Alternatively, force plate technology introduces a new level of precision and depth to the STS test as performing the FSTS on force plates can provide a range of additional insights, including:
- Time to Sit and Time to Stand
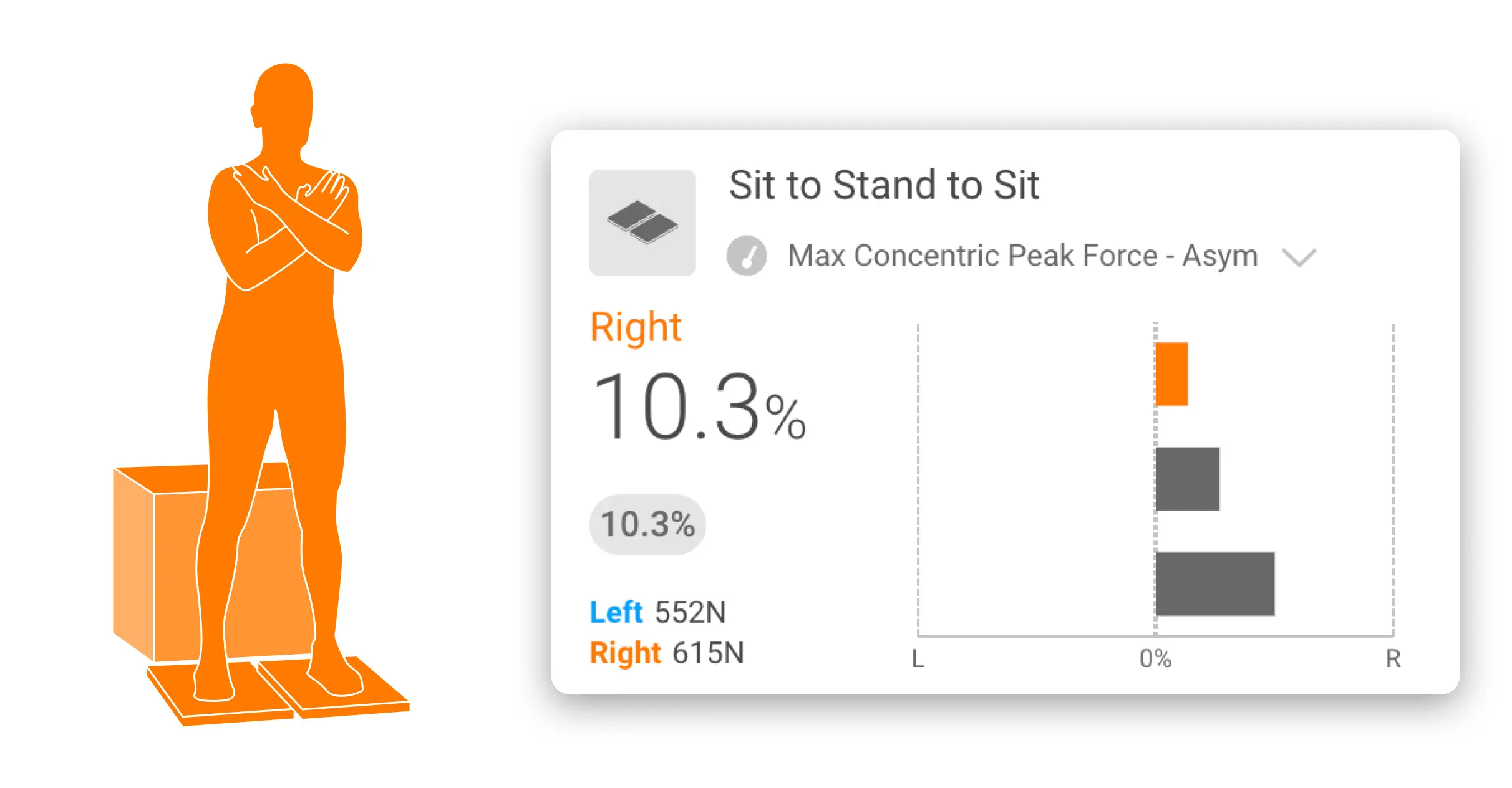
- Average standing and sitting force asymmetry
- Mean RFD
- Peak standing force and peak sitting force
- Peak standing and sitting force asymmetry
| Test | ForceDecks Metric | What it Means | Expected Progression |
| STS (with ForceDecks) | Mean Standing RFD | How quickly the client can produce force in the upward standing phase. | RFD should improve with proper training; this is a key consideration for elderly and neurologic patients. |
 | Average Standing & Sitting Force Asymmetry | How equally do they distribute force across both legs when standing up and sitting down. | Asymmetry should decrease as weight distribution becomes even between limbs. |
This shift from qualitative observation to quantitative analysis opens opportunities for a deeper understanding of physical capabilities. The value of such detailed metrics is fully realized when they are interpreted against a backdrop of established normative data, such as Norms (integrated normative data in VALD Hub) or published research, allowing for precise, tailored interventions.
Applying the 30-Second Sit-to-Stand Test (30STS)
The 30STS is best known for its use in clinical settings and has been widely researched. There are published normative data for populations such as:
- Inactive adults
- Older adults at risk of falls
- Community dwelling elderly
- Osteoarthritis patients (including hip and knee and OA patients awaiting replacements)
This assessment aims to quantify muscular endurance and capacity via a number of STS repetitions executed in 30 seconds. An increase in repetitions over time indicates an improvement in physical capacity, whereas a decrease indicates regression.
An example of the normative data for Falls Risk populations is summarized here:
Applying the 5-Repetition Sit-to-Stand Test (5STS)
The 5STS is best known for its use in stroke rehabilitation, neurological conditions and chronic disease management, and has been widely researched. The goal of the 5STS is to reduce the time taken to complete 5 repetitions. If the time is reduced, it represents positive physical progression, whereas an increase suggests regression.
Published normative data for the 5STS includes populations such as:
- Stroke patients
- Older adults and geriatric care
- Vestibular disorders
- Pulmonary diseases
- Parkinson’s disease
- Multiple sclerosis
An example of the normative data for Stroke populations is summarized here:
Functional Sit-to-Stand Test (FSTS)
Unlike the 5STS and 30STS which assess the quantity of movement, the FSTS is used by practitioners to assess the quality of movement. FSTS assesses how the individual executes the movement and typically involves a visual analysis, scoring the movement in a qualitative manner. Insights from this test can help shape intervention programs and are particularly useful in cases where there is stagnation in the other STS tests.
The FSTS is used on a wide range of populations including those mentioned previously and all aged populations following an injury or surgery, where the patient may be unable to perform a squat.
However, technology adds a new dimension to the FSTS. Technology transforms the STS movement into data and that data into actionable insights, allowing for personalized rehabilitation and exercise plans. This data-informed approach, supported by intuitive features like ForceDecks Vision, simplifies the interpretation process, making complex data accessible and actionable.
...technology adds a new dimension to the FSTS ...transforming the STS movement into data and that data into actionable insights.
By introducing force plates, a well-known and simple clinical test can yield a range of new insights.
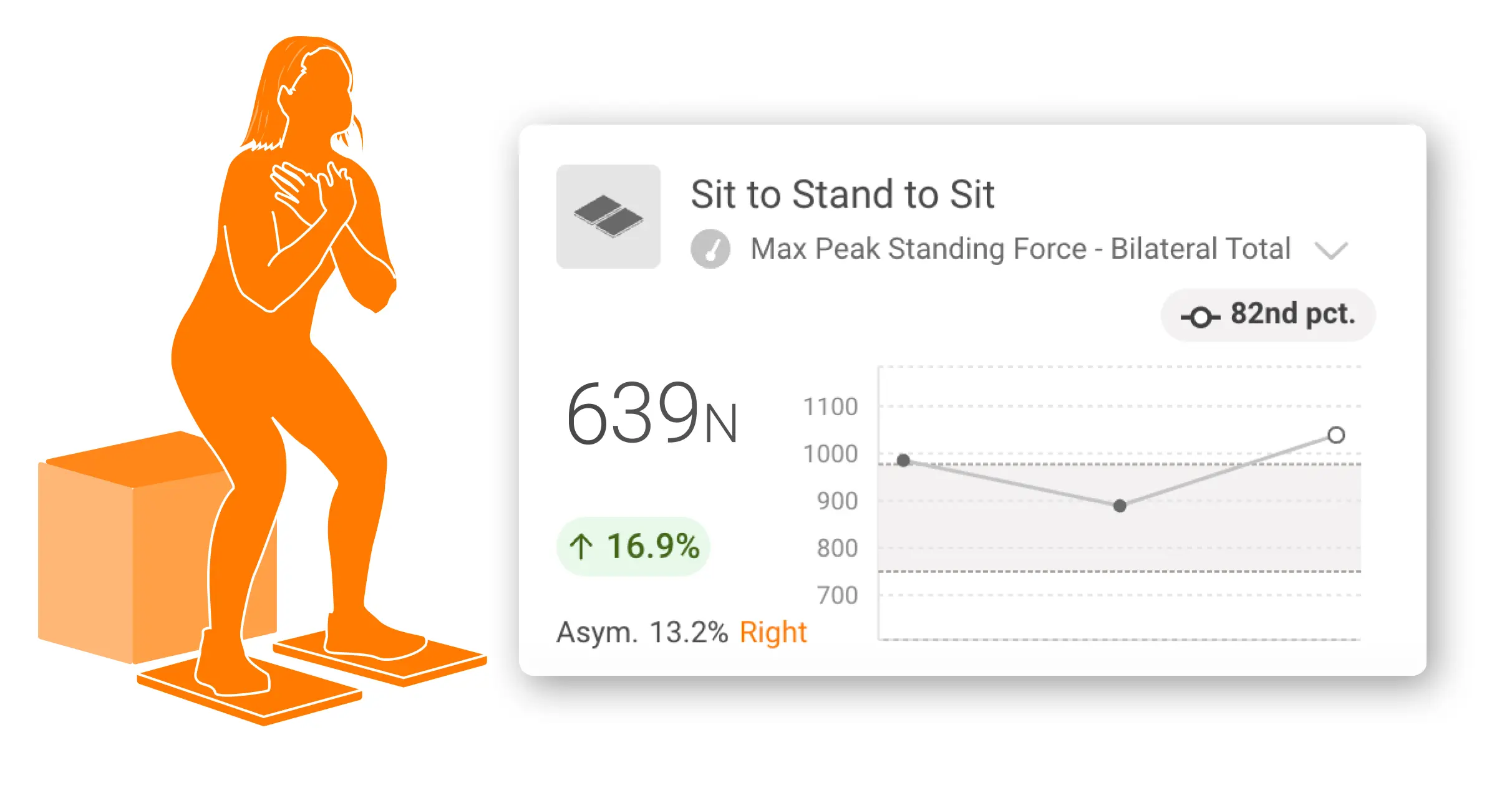
For example, if there is a clinically meaningful mean force asymmetry, this gives the practitioner insight into which limb may require particular attention in the management plan. Over time, if this metric starts to normalize, it suggests that the person’s ability to distribute weight more evenly between sides is improving. However, if asymmetry is not improving, this may indicate the need to review the intervention program rather than continuing with the same approach. As such, these metrics provide significantly greater insights into how the STS action is performed and how it changes over time, compared to the traditional metrics from the 5STS and 30STS, which focus on time and repetitions.
Further enhancing the utility of this technology, VALD’s Norms aggregate millions of data points to provide a demographic-based reference standard. This allows practitioners to position their clients' performance within a broader spectrum, comparing it against millions of other results from similar populations. Such comparisons are invaluable, offering a clear perspective on where a patient stands relative to their peers.
VALD’s Norms aggregate millions of data points to provide a demographic-based reference standard... Such comparisons are invaluable, offering a clear perspective on where a patient stands relative to their peers.
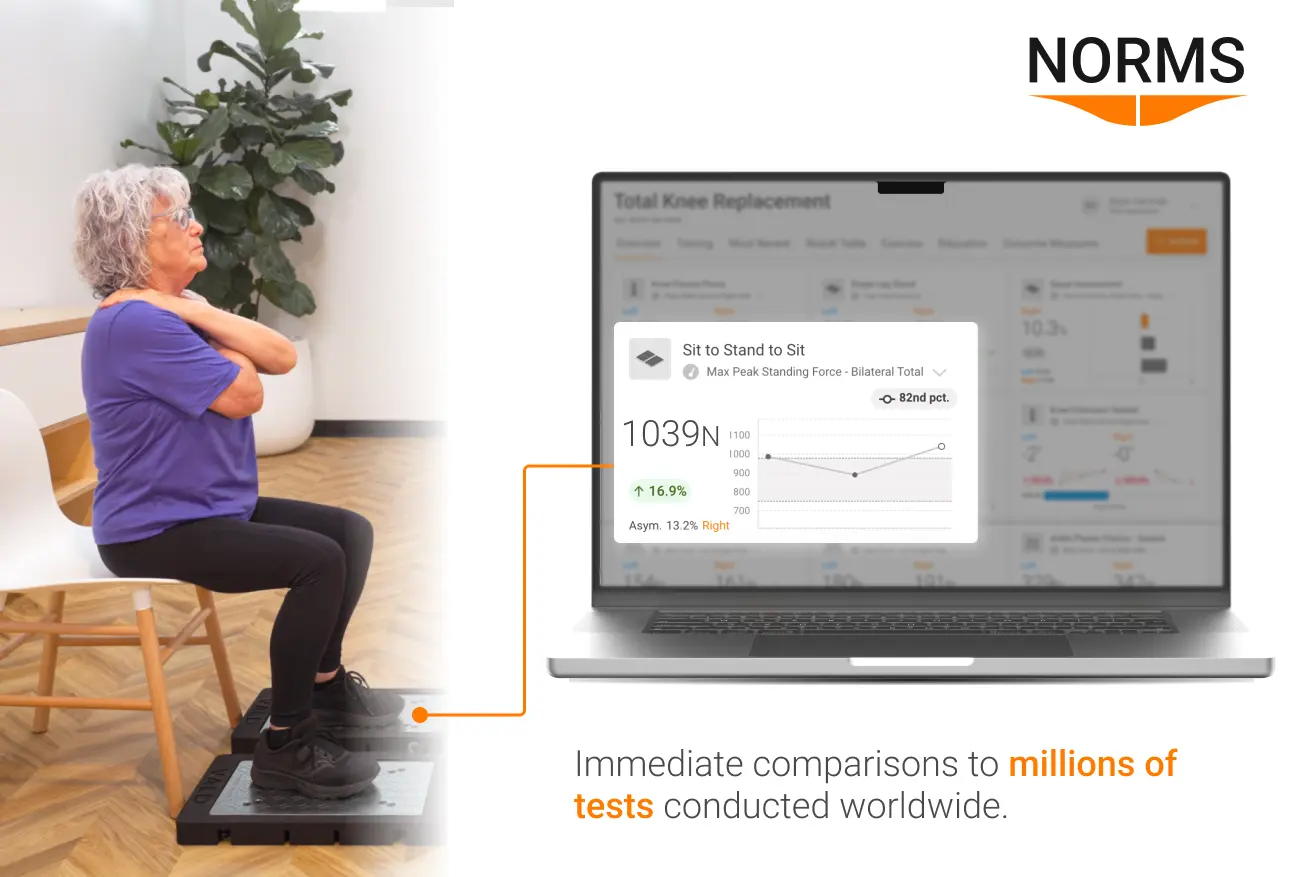
By combining detailed analysis with normative data, practitioners can conduct assessments that have enhanced accuracy which can be more meaningful. The transformative impact of technology in healthcare is highlighted by tracking progress over time, offering longitudinal data specifically for rehabilitation and physical fitness.
The transformative impact of technology in healthcare is highlighted by tracking progress over time, offering longitudinal data specifically for rehabilitation and physical fitness.

Environment and Protocol Considerations
When administering the 30STS and 5STS, there are several factors to consider ensuring accurate results and participant safety – some being:
- Appropriate chair height
- Avoiding arm support
- Maintaining proper form
- Correct foot positioning
- Consistent timing
- Monitoring for fatigue and discomfort
- Accounting for patient's limitations
- Ensuring a safe test environment
These parameters are crucial in standardizing the test for accurate comparisons. Additionally, when incorporating force plates into your testing protocol, adhering to the “Golden Rules of Testing” is important to maintain test reliability:
- Ensure a solid testing surface
- Maintain a consistent testing setup
- Zeroing the force plates before each test
- Measure weight accurately
- Follow best practice protocols
- Use consistent cues
- Require quiet periods between reps
To refine your application of force plate technology in assessments and enhance testing precision and reliability, explore our Practitioner’s Guide to Force Plates.
Ensuring Accuracy and Reliability
The technical reliability and validity of the STS test including both 30STS and 5STS have been established through extensive research, demonstrating high intra- and inter-rater reliability, making it a dependable tool in clinical settings.
Although the reliability of the STS test is robust, it is important to note that it can vary across different settings. In clinical environments, its standardized execution ensures uniformity. However, in home settings, variables such as chair height and absence of professional oversight can affect results, underscoring the importance of accurately assessing outcomes to ensure they reflect true functional ability.
Acknowledging the population-specific reliability of the STS test is imperative. Whether it is an elderly individual navigating the complexities of aging, a patient on the road to recovery post-surgery or anyone struggling with serious mobility problems – the test's reliability can provide insightful revelations. This highlights the importance of a tailored approach in functional mobility assessment to meet the individual needs of each patient.
STS test validity goes beyond just measuring strength and mobility; it can help to predict falls risk, hospitalization needs and the efficacy of rehabilitative interventions – supported by its strong correlation with other established measures of lower limb strength and functional mobility. Moreover, its consistent reliability, with test-retest scores typically above 0.8 (on a scale where 1 is perfect reliability), and its correlation with other mobility metrics underscores its potential to enable preventative strategies and informed decision-making – making it an invaluable tool in clinical settings.
...beyond just measuring strength and mobility, the STS test can help predict falls risk, hospitalization needs, and the efficacy of rehabilitative interventions ...making it an invaluable tool in clinical settings.
Training Considerations and Progressions
The STS test is not only a powerful tool for assessing lower-body strength and endurance but also serves as an effective training method. Emphasizing proper technique, gradual progression and tailored approaches is essential for optimizing health outcomes and ensuring safety.
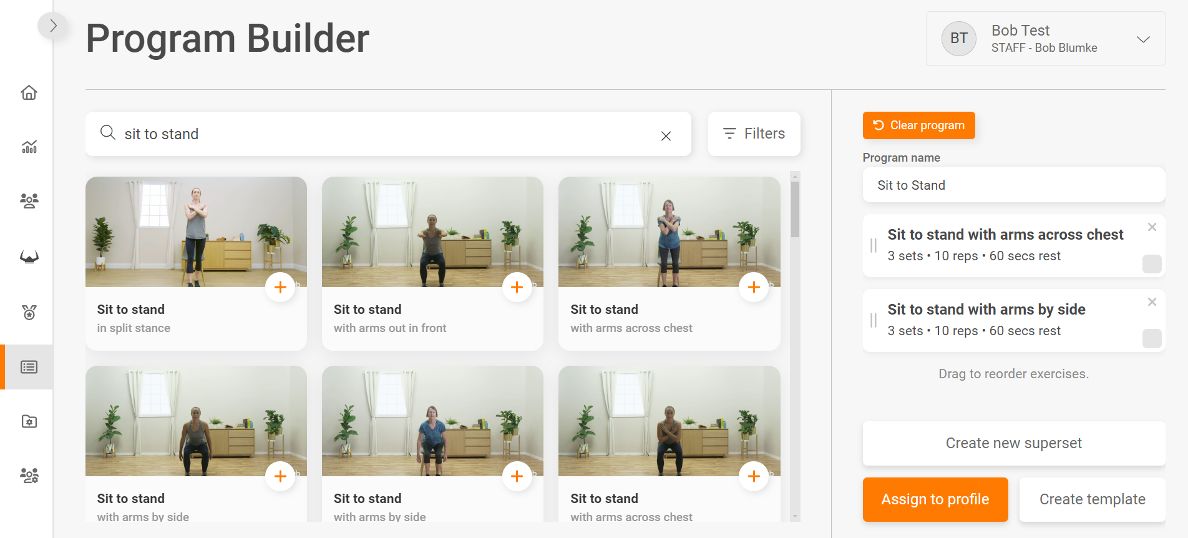
Performing STS training on ForceDecks provides immediate insight and biofeedback through data visualization. Furthermore, exercise prescription software such as TeleHab can be utilized to provide and monitor tailored intervention programs.
The integration of technology in functional mobility assessments, such as the STS test, is highlighted through impactful real-world cases where ForceDecks provided valuable insights beyond traditional metrics of time and repetitions.
This approach yields not only better results but also a shift towards more informed, hyper-personalized rehabilitation strategies. This evolution, strengthened by expert insights and normative data, illustrates technology's impact on healthcare.
If you would like to know more about how to integrate VALD’s human measurement technology into your practice or organization to help with more in-depth assessment much like the STS test, please reach out here.